Lives Lost Amid ER Violations, Investigation Finds

Randy Strickland, shown with wife, Mary, died after North Metro Medical Center in Jacksonville, Arkansas, failed to follow standards of care established by the federal Emergency Medical Treatment and Labor Act, records show. WebMD and Georgia Health News analyzed 10 years of EMTALA violations by hospitals around the United States from March 2008 to March 2018.
Photo courtesy of Georgia Health News
By Brenda Goodman and Andy Miller
This special report, Deprived of Care: When ERs Break the Law, is an investigation by WebMD and Georgia Health News.
Randy Strickland walked into the ER at North Metro Medical Center burning with fever and trembling. He told the man and the woman who were staffing the triage desk that he was nauseated and felt like he needed to throw up.
The emergency room was nearly empty. Randy was a volunteer at the hospital in Jacksonville, Arkansas, and hoped he would get home quickly.
But repeated visits by his wife, Mary, and son James to the triage desk didn’t bring Randy any closer to getting care. Over the next two hours, he lost his ability to speak or respond to questions. His breathing became labored. Finally, on a trip to the bathroom, his legs buckled as he clutched Mary’s arm for support.
“I can’t hold him up!” Mary yelled as she pounded on the wall that separated the bathroom from the triage desk, trying to summon the ER attendants.
When no help came, James picked up his phone and dialed 911. Could they take his dad to a different ER? he asks the operator, according to a transcript of the call.
“I’m sorry sir, my ambulance will not respond to a hospital,” the operator responds. “Have you tried talking to them or anything?”
“It’s just — I don’t know what they’re waiting for,” James says.
After a pause, the dispatcher asks if they can get Randy out to his car in the parking lot, where paramedics can pick him up.
James and Mary wheeled Randy outside in a drenching rain and slid him into the back seat of their gray Toyota RAV4.
When the paramedics pulled up, Mary says, they knew immediately that Randy was too sick to be taken to another hospital. They took him back into the ER through an entrance used by ambulance crews, and the hospital’s medical teams finally jumped into action. But by that time, Randy was critically ill.
A team of doctors and nurses struggled for about an hour to save him.
Finally, a doctor came to speak with Mary.
“Is he gone?” Mary asked.
“He is, but we’re going to do CPR until you tell us to stop,” he told her.
Randy Strickland died after North Metro failed to follow standards of care established by the federal Emergency Medical Treatment and Labor Act, or EMTALA, records show. Investigators cited the hospital for failing to keep adequate records on Randy and for failing to do an appropriate medical screening exam.
Administrators at North Metro Medical Center and its parent company, Allegiance Health Management, based in Shreveport, Louisiana, declined to comment on the EMTALA citations.
Though EMTALA has been on the books for more than 30 years, hospitals are still violating it hundreds of times a year, sometimes with devastating results for patients.
WebMD and Georgia Health News analyzed 10 years of EMTALA violations by hospitals around the United States from March 2008 to March 2018. The records, obtained under a Freedom of Information Act request, show cases where complaints were substantiated by investigators for the federal Centers for Medicare and Medicaid Services, meaning the hospital was found to be at fault. Our investigation found:
- More than 4,300 violations from 1,682 hospitals in total over 10 years.
- Violators represent about a third of the nation’s approximately 5,500 hospitals, according to statistics from the American Hospital Association.
- Hospitals in the Southeast accounted for 1,175 violations over 10 years, more than any other region.
- Florida was the worst state in the nation for the number of violations, followed by Texas, Pennsylvania, New York, California and Georgia.
- Smaller hospitals — those with fewer than 100 beds — accounted for the largest number of violations — 1,488, or 34 percent of the total.
- Failure to do a thorough medical screening exam was the most common violation committed by hospitals, accounting for more than 1,300 citations, nearly twice as many as the second most common violation: transferring patients inappropriately.
- In a deeper analysis of investigation reports from January 2016 to March 2018, at least 34 patients died during that period after emergency departments violated the law.
- A medical condition often cited in these violations was pregnancy. About 1 in 12 involved women who were pregnant or in labor. About 1 in 7 involved patients who were having a mental health crisis, including having suicidal thoughts.
While violators over the 10 years represent about a third of hospitals across the United States, the chances of any individual trip to the ER resulting in a documented violation are very low. In 2016, for example, there were just 459 EMTALA violations across the country out of 142.6 million emergency room visits, according to the American Hospital Association.
Yet experts say the raw numbers belie both the scope and severity of the problems they see. That’s because enforcement of the law depends on someone filing a complaint. Although anyone can file a complaint, it’s most often a doctor, nurse, or hospital administrator.
Howie Mell, an emergency doctor in Chicago and a spokesman for the American College of Emergency Physicians, says that when someone from a hospital makes a complaint about what happened at another hospital, both hospitals are investigated. While complaints are anonymous, investigations can be rigorous, and they often catch smaller violations — like failing to post signs about patient rights in an emergency room — along with larger ones that directly affect patient care.
“That system of going after both sides really discourages people from complaining,” says Mell.
Given that fact, he says, when you do see an EMTALA violation recorded in the system, it’s usually because something really serious happened.
“They were either really egregious, or what you’re seeing is the tip of the iceberg” for that hospital, Mell says.
When Hospitals Fail Patients
EMTALA, signed into law by President Ronald Reagan in 1986, was designed to prevent the practice of so-called wallet biopsies — where hospitals would turn away patients who couldn’t prove they had financial resources like health insurance to pay for their care. Those patients ended up at public hospitals, often in unstable conditions. They died about three times more often than patients who were not transferred this way, according to an influential 1986 study on the practice.
While this kind of patient dumping still happens, it appears to be far less common than it used to be.
Instead, our investigation found that many hospitals seem to be breaking the law because they lack the resources to provide the level of care the law requires.
“The problem is that the majority of the EMTALA fines that are out there are not egregious money-grubbing things. They are not wallet biopsies. They are literally the emergency room or the staff of a hospital running up against a lack of resources,” says Mell.
Other experts agree.
“An EMTALA [violation] usually implies you don’t have the resources to take care of the patient at your facility. Smaller hospitals have fewer resources,” says Boykin Robinson, an emergency doctor who runs the Atlanta-based Core Clinical Partners, a company that staffs emergency rooms.
Our data analysis found that hospitals that violate EMTALA are most likely to be smaller hospitals, or those with fewer than 100 beds. They accounted for 1,488 violations over the decade, more than any other group. According to statistics from the American Hospital Association, hospitals with fewer than 100 beds accounted for about half of all hospitals in the U.S. in 2016.
That makes sense to Ryan Kerr, a former nurse and an attorney with Arnall Golden Gregory, a law firm that consults with hospitals.
He says smaller hospitals often lack services to fully examine or stabilize emergency patients. Under the law, that means they may need to transfer patients more often, a process that can easily go awry.
“Each of these transfers create an opportunity for the hospital to inadvertently violate EMTALA if the hospital could have stabilized the patient or the hospital committed an error in the transfer process,” Kerr says.

That’s what happened to Theresa Kuhn, 58, a nurse and high school health sciences teacher from Social Circle.
Kuhn had a routine outpatient procedure on Friday, Dec. 11, 2015, to look for the cause of some post-menopausal bleeding.
By Sunday morning, she was in unbearable pain. Her doctor’s office advised going to the closest emergency room.
That was at Piedmont Newton Hospital, a 103-bed hospital in nearby Covington. To take her to Gwinnett Medical Center, the hospital system that had originally treated her, would have taken them another hour, says her ex-husband Brian Kuhn, who drove her to the hospital.
An X-ray performed in the emergency room at Piedmont Newton revealed a puncture in her bowel that was leaking into her abdomen. A doctor in the ER told Theresa she needed surgery.
But they waited. And waited.
Brian says he knew that was dangerous. He asked the nurse, “Well, if she has a hole poked in her bowel and the fluid comes out — isn’t that poisonous?”
“Yes,” she said.
“Shouldn’t we be concerned about time?” Brian asked.
Eventually, another doctor, the hospital surgeon, came to speak to them. She told Brian she had been making arrangements to transfer Theresa to the 500-bed Gwinnett Medical Center in Lawrenceville for her urgently needed surgery.
Brian was stunned. A medical helicopter came to pick up Theresa. It was 5:30 p.m. By that time, she had spent nearly four hours in the Piedmont Newton ER.
Theresa vomited midflight, sending stomach contents into her lungs and worsening her condition.
The doctor who did her original procedure met Brian and Theresa’s daughter, Lauren, and told them he was going to rush Theresa into surgery. They removed part of her colon and took out the surrounding infection. Brian says the doctor told them the surgery went well.
But Theresa never woke up. Hooked up to a ventilator and in septic shock, she died the next day.
Federal investigators cited Piedmont Newton for failing to stabilize Theresa and for transferring her to another hospital even though it wasn’t safe to move her. In their report on the case, investigators determined the surgeon who transferred Theresa had the skill and resources to perform the needed operation. In an interview with investigators, the surgeon says in her 34 years of practice, she’d never heard of EMTALA and wasn’t familiar with the law, records show.
Piedmont Healthcare, which acquired the Newton hospital just months before the incident, declined to comment on the specifics of Theresa’s case or the violations they were cited for as a result.
Like the other families interviewed for this story, Theresa’s relatives had no idea that her case had been the subject of a federal investigation.
“I felt in my heart that this was 100 percent preventable,” says Sarah Homer, Theresa’s sister who lives in Tampa, Florida. She’s taking care of Lauren, who was in college when Theresa died.
“The delay in treatment was just shocking to us,” she says.
‘No Physician Available’
Small hospitals are more likely to serve more rural populations. They’re also more likely than larger hospitals to be financially fragile, says Jimmy Lewis, CEO of HomeTown Health, an association of rural hospitals in Georgia and Florida.
At Hill Hospital of Sumter County in York, Alabama, a rural community just across the state line from Mississippi, federal investigators found an envelope labeled N.P.A. — for “No Physician Available.” It contained records on 38 patients who came to the emergency room for help when there was no doctor there to treat them at the 27-bed facility. The cases, which included two deaths, spanned a four-month period from 2017 to 2018. The violations were so serious, the federal government threatened to end the hospital’s contract with Medicare, though that didn’t happen.
One of those patients was Quarmaine Seals, a 25-year-old truck driver and father of two young children. He was also a motorcycle enthusiast. According to a police report, he was riding a motorcycle down a two-lane highway in York the night of Sept. 1, 2017, when a car backed out of a driveway onto the rural road in front of him. The police report estimates Seals was traveling 100 mph in a 35-mph zone. He struck the passenger side door and flew 30 feet over the car. Witnesses found him thrown into the bushes, his body wrapped around a metal hand railing along the walkway to a house.
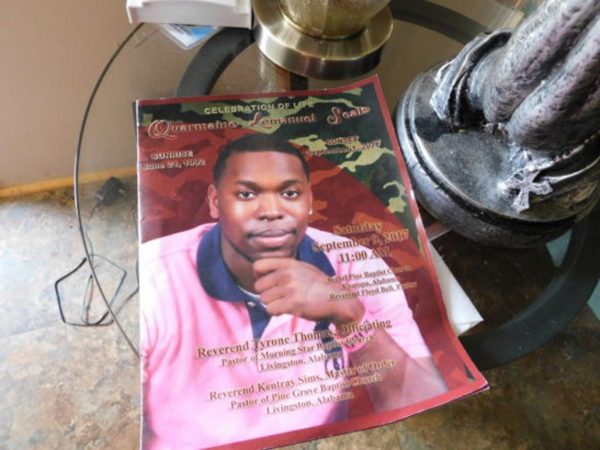
Paramedics showed up within 10 minutes and took Seals to the closest emergency room at Hill Hospital, where there was no doctor to treat him. An air ambulance was dispatched from Mississippi to pick him up from Hill Hospital, according to federal records
While EMTs waited for it to arrive, they tried to revive Seals in a trauma room at the hospital.
He was pronounced dead over the phone by the doctor who was remotely directing the air ambulance crew.
In this small town, where everyone knows everyone else, Willie Seals, Quarmaine’s mother, had been called about the accident and was already at the hospital when they wheeled her son’s broken body into a trauma room.
The stress of seeing him caused her to collapse. Paramedics loaded her into an ambulance and drove her to the next closest hospital, in Meridian, Mississippi, for care.
“They took me, but they didn’t take him,” she says. “I got the ambulance ride he should have had.”
“It destroyed me because I felt like had a doctor been there, they could have done more for my son.”
A year after the accident, she still dreams about Quarmaine. She cries in her sleep.
“Not a day goes by when I don’t miss my son. He was only 25. He wasn’t through living.”
Gena Springfield, a former nurse who worked at Hill Hospital off and on for two to three years, says the hospital was having trouble paying its staff, even as far back as 2014, when she was there.
“That’s why I quit working there, because they couldn’t pay the nurses, they couldn’t pay the doctors. We didn’t have the things we needed to work there with. I mean, it was dangerous,” she says.
Federal investigators concluded that conditions at the hospital placed patients in “immediate jeopardy.” They gave the hospital 90 days to improve or lose federal funding, a move that almost certainly would have meant its closure. The hospital has since been taken off the immediate jeopardy list.
When asked why the hospital had struggled to keep a doctor in its ER, administrator Loretta Wilson declined to comment on the specifics of the violation.
In general, she says Hill Hospital faces many of the same challenges as other small, rural hospitals.
“We have a lot of people who come to our hospital who can’t pay. We have to provide these services. Nobody pays for that. We don’t have the population with access to insurance,” Wilson says.
Wilson also says staff had cut their own salaries just to keep the hospital running.
But federal regulations require hospitals that take reimbursements from Medicare or Medicaid to offer a certain level of care in emergencies.
When resources fall short, they’re supposed to notify CMS and local ambulance crews that they can’t take emergency patients. They’re also supposed to post a public notice. Hill Hospital failed to do that.
In Quarmaine Seals’ case, no one had told the paramedics who brought him to the hospital that it didn’t have a doctor available.
Problems like those at Hill Hospital show what some people call a downside of the law. Hospitals are required to serve everyone whether they can pay or not.
“Care can be quite expensive, and there’s no money that would pay for that care, which is required. That’s where we get into the unfunded mandate. We agree with the mandate; we just think there ought to be funds available to pay for it,” says Michael Carius, MD, a spokesman for the American College of Emergency Physicians, or ACEP.
ACEP has worked with Congress to introduce two bills to try to relieve some of the financial pressure that the law creates for hospitals. The first would create a way to get the government to reimburse hospitals when they provide care that isn’t paid for. The second approach, which is less direct, would shield doctors who treat ER patients from lawsuits, Carius says.
But so far, neither of the bills has gained any traction in Congress.
Feds Step Up Enforcement
Cheryl Fish-Parcham, director of access initiatives for the nonprofit advocacy group Families USA, says that EMTALA has largely been forgotten.
“I think it’s really important that there be strong enforcement of this law because consumers are not in a position to enforce this themselves,” she says.
Before 2015, fines levied under EMTALA had been authorized under the Social Security Act and were exempt from adjustment for inflation. That means in 30 years, they’d never gone up, says April Washington, a spokeswoman for CMS. Each violation could cost a doctor or hospital up to $50,000. The penalty for hospitals with fewer than 25 beds was $25,000 per violation.
In 2015, Congress passed the Federal Civil Penalties Inflation Adjustment Act, which effectively doubled EMTALA and other civil fines “to maintain their deterrent effect,” says Washington.
Now, doctors and hospitals face up to $104,826 for each violation.
The adjustment recently resulted in the largest fine ever levied against a hospital for an EMTALA violation — nearly $1.3 million. The nonprofit AnMed hospital system, which serves South Carolina, settled with the Justice Department after investigators found the three hospitals were “boarding” dozens of mental health patients in their emergency room for as long as 38 days when they had open psychiatric beds at the same facilities. The patients had been involuntarily committed. The hospital had a longstanding policy of transferring involuntarily committed patients to the state psychiatric hospital, rather than accepting them to their in-house psychiatric unit, according to news reports. The state mental hospital was short of space, prompting long waits for transfer.
AnMed launched a plan of correction in 2015, which was accepted by CMS. The plan called for adding security and making structural changes to its own behavioral health unit so that it could accept involuntarily committed patients, according to a hospital statement. They also added staff, gave existing staff more training, and came up with new ways for doctors to care for involuntarily committed behavioral health patients, the statement says.
“AnMed Health continues to work with state and local mental health agencies to improve health care for the behavioral health population,” according to a written statement.
The massive fine was seen by some health law experts as a warning to hospitals that CMS was beefing up its response to hospitals that don’t follow EMTALA when it comes to mental health.
Jay Bhatt, senior vice president and chief medical officer at the American Hospital Association, says hospitals take the law “very seriously.”
“Hospitals strive to stabilize and treat all patients with emergent medical needs. When a hospital does not have an available bed or does not offer the treatment a patient needs, it will transfer the patient to another hospital that does have the capability,” Bhatt says. He says that it can sometimes be challenging to find the right treatment facility.
Washington of CMS says the federal agency is looking at other ways to boost EMTALA enforcement, too. For example, most cases are investigated and enforced by state health care regulators that contract with the federal government. That’s not always an effective system, especially if state regulators are too stretched or too intimidated by their local hospitals to offer strong enforcement.
To remedy that, CMS administrators are proposing new federal teams to help state survey agencies with difficult cases. These teams would also help educate and rehabilitate failing hospitals.
“EMTALA is fundamentally the Golden Rule of emergency care, codified by Congress,” says Richard Wild, a CMS regional chief medical officer. “Every hospital should strive to provide every person who presents symptoms in an emergency department with the best care. There should be one standard of care — their best care.”
But for now, patients wouldn’t necessarily know they’ve arrived at a struggling facility until it’s too late.
North Metro, the hospital where Randy Strickland died, is a 64-bed hospital in Jacksonville, Arkansas, a suburb about 20 minutes northeast of Little Rock.
Once a vital part of the town, the facility has fallen on hard times in recent years. The hospital owes millions to the federal government for back taxes and fraudulent Medicare billing, and it faced several lawsuits from vendors who were not paid. Staff turnover has been high. The hospital has had six CEOs in the last five years and a string of medical chiefs of staff.
Medicare’s Hospital Compare website gives the hospital 1 out of 5 stars for quality. It lags state and national averages for several measures of “timely and effective care.” At North Metro, for example, patients with chest pain wait an average of 70 minutes before they get an EKG — a test that helps to diagnose a heart attack. In the rest of the state and nation, patients with chest pain wait an average of just seven minutes before they get that test, the data show.
Only 3 percent of patients treated at North Metro received the right care for sepsis or septic shock, compared with 47 percent of such patients in Arkansas and 49 percent of patients nationally.
Tracy Phillips, was the hospital’s chief of staff when he treated Randy Strickland the night he died. Phillips says he was at a concert when he got a call from a doctor on duty that he needed help with a patient. He says he was at the hospital within 10 minutes.
Phillips was eventually able to put a tube down Randy’s throat to help him breathe and insert an IV, but those measures came nearly three hours too late.
“He was septic,” Phillips says in a recent interview. “It was septic shock.”
“My first question was, ‘What took so long?’ ” Phillips says. “That’s when I started investigating it.”
There was a mistake made. That should never, ever, ever have happened. Ever.
North Metro’s former chief of staff Tracy Phillips, who says he changed ER triage procedures after Randy Strickland’s death
The clerk at the front desk had told James, Randy’s son, that they couldn’t take Randy back because they were attending to a priority patient.
But Phillips, who left North Metro in December 2017, says his investigation found that there was no priority patient.
The nurse on duty had left early — about a half-hour before the end of her shift — without telling anyone, Phillips says.
The ER clerk and another woman who was staffing the reception desk had failed to recognize how sick Randy was.
The ER doctor did not know the situation because Randy was not sent to a room in the back to be seen.
After Randy’s case, Phillips says he changed ER triage procedures so that patients with low blood pressures or rapid heart rates were brought straight back to see a doctor.
“They just didn’t bring the guy back. They didn’t think he was that sick,” Phillips says.
“There was a mistake made,” he says. “That should never, ever, ever have happened. Ever.”
Coming Next Week: A focus on pregnancy and mental health cases
Brenda Goodman is a staff writer for WebMD. Her work has appeared in The New York Times, Scientific American, Psychology Today, The Boston Globe, Self, Shape, Parade, U.S. News and World Report, and Atlanta Magazine. She has a master’s degree in science and environmental reporting from New York University.
Andy Miller is editor and CEO of Georgia Health News
Your Rights In The ER
The Emergency Medical Treatment and Labor Act, or EMTALA, guarantees a certain level of medical care to anyone who comes to an emergency department that accepts payments from Medicare or Medicaid.
Some labor and delivery units and psychiatric hospitals are also governed by EMTALA.
Under the law enacted in 1986, emergency departments must:
- Offer patients a timely and appropriate medical screening exam.
- This exam is different from triage, in which a nurse or other provider takes vital signs to decide the order in which to see patients.
- Unlike with triage, a health care professional with a certain level of expertise — typically a doctor, advanced practice nurse, or physician assistant — must do the medical screening.
- Medical screening exams are done to find out the cause of a patient’s symptoms. They cannot be delayed or denied in order to ask about a patient’s ability to pay.
- Medical screening exams must make use of all the hospital’s relevant resources, for example, lab tests or CT scans.
Over the last 10 years, the most frequent EMTALA violation by hospitals was the failure to do an adequate medical screening exam.
- Stabilize patients who have emergency medical conditions.
Failure to offer stabilizing treatment was the fourth most common EMTALA violation over the last 10 years.
- If a hospital can’t stabilize a patient, it is required to arrange an appropriate transfer to another facility, including:
- Treatment to lessen the risks of transfer
- Getting consent from the receiving hospital to accept the transfer
- Ensuring the transfer involves qualified personnel and transportation (an ambulance)
Failure to do an appropriate transfer was the second most common way hospitals have violated EMTALA over the last 10 years.
- Keep appropriate records on patients, including a central log of who came to the ER and what happened to them.
Failure to keep this log was the third most common EMTALA violation over the last 10 years.
- Post signs in the ER letting people know about these rights.
- Keep a list of on-call doctors who can see patients in case of an emergency.
- Accept appropriate transfers from other hospitals if the receiving facility has special abilities or is able to care for an incoming patient.
- Not punish any hospital employee who reports a violation.
- Report any improperly transferred patients it receives within 72 hours.
SOURCES:
Centers for Medicare and Medicaid Services, State Operations Manual, Appendix V, Interpretive Guidelines, Responsibilities of Medicare Participating Hospitals in Emergency Cases, 7-16-10.
Editor’s note: If you have experienced what you think may be an EMTALA violation, you can contact your regional Centers for Medicare & Medicaid Services office. You can find your local office from the CMS.gov website. Anyone can report a violation anonymously. The CMS office will need details to properly investigate your claim. Health officials will investigate your claim, but no more involvement is likely necessary on your part, CMS officials say.
How We Reported This Story
For this eight-month investigation, WebMD and Georgia Health News filed a Freedom of Information Act request to the Centers for Medicare & Medicaid Services for a list of all EMTALA violations by hospitals across the U.S. between January 2008 and March 2018.
The list detailed the number of violations, which hospitals had committed them, when they happened, and the nature of the offenses.
There were 4,341 violations by 1,682 hospitals. That’s almost a third of about 5,500 registered hospitals in the United States, according to the American Hospital Association.
We partnered with the geographic information systems company Esri to map this data and analyze it in different ways. That analysis revealed that smaller hospitals — those less than 100 beds — were more likely to have an EMTALA violation. We used the American Hospital Directory for bed size data.
Because we wanted to understand more about what was behind these violations, we also requested the investigation reports for the most recent 27 months of violations. These reports included full details on 874 EMTALA violations with more than 1,400 pages of documentation.
We used the facts from these investigation reports, which do not include names of patients and other details, to help us find patients and families that were affected by these violations. In some cases, we found police reports, medical records, and, in one instance, a 911 call to give more details, and we did interviews with family members and medical personnel.
We welcome questions or feedback at bgoodman@webmd.net and amiller@georgiahealthnews.com.
Valarie Basheda and Aaron Gould Sheinin contributed to the reporting.
SOURCES:
Centers for Medicare & Medicaid Services.
American Hospital Association.
American Hospital Directory.
Tips For Emergency Care
By Andy Miller
If you believe your life or someone else’s life is at risk, you should call 911 rather than driving yourself or getting someone else to drive, emergency medicine physicians say.
“Trust the EMS professionals and system in your area to get you to the most appropriate hospital as quickly as possible,” says Dr. Brad Uren, assistant professor of emergency medicine at the University of Michigan Medical School and a spokesman for the American College of Emergency Physicians.
EMS can evaluate patients and begin treatments that can save lives, he adds.
Examples of such life- or limb-threatening conditions include large severe burns, serious bleeding, severe chest pain or shortness of breath, severe headaches, sudden vision changes, weakness of arms or legs, or severe trauma where a person is unconscious or not acting normally.
If you choose to seek care on your own in such an emergency, the closest hospital is always the appropriate hospital, Uren says.
Of course, people in rural areas may have only one hospital ER available.
“If you end up in a place that can’t definitively take care of you, they should be able to get you somewhere that can,’’ says Dr. Boykin Robinson, an emergency medicine physician who runs an ER staffing company in Atlanta.
For a patient who has already been evaluated by EMS professionals and judged stable, offering a choice of ERs to patients makes sense, Uren says.
For less grave health conditions, though, people can do homework on medical quality to determine which ER to pick, says Leah Binder, president and CEO of the Leapfrog Group, an organization that rates hospitals for patient safety.
“The time to select an ER is not in an emergency,’’ Binder says. “Think about it in advance on where you should go’’ in case of a less serious emergency.
Besides Leapfrog Group’s safety ratings, Hospital Compare, created by the federal Centers for Medicare & Medicaid Services, has a category for emergency medicine.
Urgent care centers may be the right choice for problems that don’t qualify as emergencies — such as flu, fever, earaches, nausea, rashes, animal and insect bites, minor bone fractures and minor cuts requiring stitches.
Here are some websites that can help guide you in an emergency:
From the American College of Emergency Physicians:
When to Call 911 http://www.emergencycareforyou.org/emergency-101/when-to-call-911/#sm.000001mf14as6wfpdvym2nxxfd7vy
10 Tips for Moms http://www.emergencycareforyou.org/globalassets/ecy/media/pdf/acep_ecfy10tipsformoms_poster_final1.pdf
From Leapfrog:
Your hospital’s safety grade http://www.hospitalsafetygrade.org/your-hospitals-safety-grade
Staying safe at the hospital: http://www.hospitalsafetygrade.org/what-you-can-do-to-stay-safe
From CMS:
Hospital Compare: https://www.medicare.gov/hospitalcompare/search.html
Sources for ‘Lives Lost’:
Mary Strickland, wife of Randy Strickland, Jacksonville, Arkansas.
Centers for Medicare & Medicaid Services, Statement of Deficiencies, North Metro Medical Center, May 24, 2017.
City of Jacksonville, recording of 911 call, April 26, 2017.
Centers for Medicare and Medicaid Services, Freedom of Information Act request, March 20, 2018.
American Hospital Association, Hospital Statistics, 2018.
Howard K. Mell, MD, spokesman, American College of Emergency Physicians, Chicago.
CMS.gov: “Emergency Medical Treatment and Labor Act,” accessed Nov. 13, 2018.
New England Journal of Medicine: “Transfers to a Public Hospital.”
Boykin Robinson, MD, emergency doctor, Core Clinical Partners, Atlanta.
Ryan Kerr, attorney, Arnall Golden Gregory, Atlanta.
Brian Kuhn, Theresa Kuhn’s ex-husband, Conyers, Georgia.
Sarah Homer, Theresa Kuhn’s sister, Tampa, Florida.
Gena Springfield, former nurse, Hill Hospital, York, Alabama.
Loretta Wilson, administrator, Hill Hospital, York, Alabama.
Jimmy Lewis, chief executive officer, Hometown Health, Atlanta.
Centers for Medicare & Medicaid Services, Statement of Deficiency, Piedmont Newton Hospital, Covington, Georgia, Jan. 13, 2016.
Willie Seals, Quarmaine Seals’ mother, York, Alabama.
Centers for Medicare & Medicaid Services, Statement of Deficiency, Hill Hospital of Sumter County, York, Alabama, Jan. 18, 2018.
Michael Carius, MD, spokesman, American College of Emergency Physicians.
Cheryl Fish-Parcham, director of access initiatives, Families USA.
Jay Bhatt, chief medical officer, American Hospital Association.
Richard Wild, MD, Centers for Medicare & Medicaid Services, regional chief medical officer, Region 4, Atlanta.
April Washington, spokeswoman, Centers for Medicare & Medicaid Services, Region 4, Atlanta.
Centers for Medicare & Medicaid Services, Hospital Compare, Accessed Nov. 12, 2018.
Tracy Phillips, DO, hospitalist physician, Redfield, Arkansas.
This article originally ran on the Georgia Health News website





