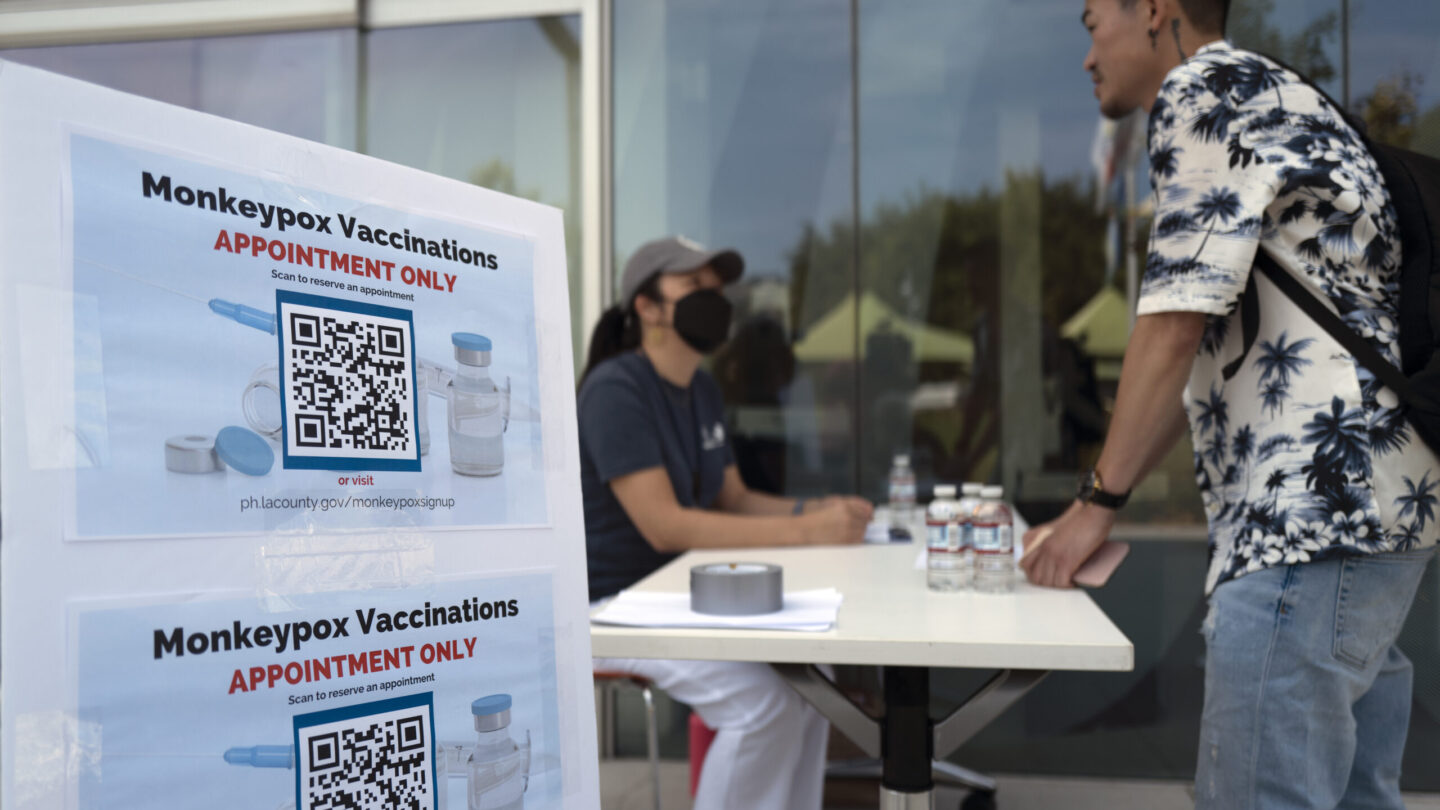
After a bumpy start, the Biden administration is trying to smooth out the vaccination campaign aimed at controlling the country’s growing monkeypox outbreak.
The effort now rests on a new and untested strategy of dividing up what were previously full doses in order to stretch the limited stockpile of vaccines in the U.S.
This comes as monkeypox cases have climbed well above 14,000 in the U.S. – a case count higher than any other country in the world – and yet many local health departments still report not having enough vaccines to reach all those who are considered at heightened risk of contracting the disease.
“We are definitely in what we’re still calling ‘The Hunger Games’ phase of this – where there’s nowhere near enough doses for the demand,” says Dr. Mark Del Beccaro, Assistant Deputy Chief for Public Health – Seattle & King County.
Already facing the expected logistical hurdles of running a vaccine campaign in a public health emergency, health officials now have to tackle another challenge: how to squeeze five doses out of single-dose vials.
“It’s great that we are able to increase the number of people we can vaccinate with the current supply,” says Claire Hannan, head of the Association of Immunization Managers. Still, “when you make a change like that, it’s kind of like turning the barge around in the middle of the sea.”
The change poses challenges with messaging and logistics – training providers and getting the right equipment – and it raises concerns among some over equity as early vaccine data rolls in, showing significant racial disparities.
Stretching a limited supply
The U.S. government’s plan to get the disease under control is largely based on giving out the JYNNEOS vaccine, a two-shot series against monkeypox made by Bavarian Nordic.
But a series of missteps at the start of the response left the U.S. with a major vaccine shortage. The federal government was slow to order vaccines, allowing other countries to jump the queue, and distribution has been chaotic for states and cities.
So far, the U.S. has shipped around 700,000 vials of the monkeypox vaccine to states and territories for distribution. The Centers for Disease Control and Prevention has said the first priority is to vaccinate the 1.7 million people who are considered at highest risk.
Facing a shortage in vaccines, the Food and Drug Administration authorized a new dosing strategy last week: the vaccine can now be administered using an “intradermal injection” – where the vaccine is injected into the skin – rather than the typical method of injecting into the layer of fat underneath the skin.
“This action serves to markedly increase vaccine supply,” said Dr. Rochelle Walensky, director of the CDC, in a video released this week. “Intradermal administration of the JYNNEOS vaccine allows vaccine providers to administer a total of up to five separate doses from an existing one-dose vial.”
Federal officials are adamant that this smaller amount of vaccine should not be considered a “partial dose” because it’s still able to produce a similar level of immunologic response as the original method of administering the vaccine.
However, the evidence for this method is scant, though it has worked for vaccinating against other diseases.
The theory rests on the fact that there are many immune cells embedded in the skin. “When a vaccine is given into this tissue, you can generate a robust immune response using a smaller amount of vaccine,” said Dr. John Brooks, a medical epidemiologist from CDC in the video, citing a 2015 study on the vaccine. Brooks also stressed that the method has been studied on other vaccines including those for flu and rabies.
One vial equals five doses? Not so fast
There’s also a practical problem with the plan to squeeze five doses out of what was once a single dose:
“It’s just mechanically difficult to do,” says Del Beccaro of Seattle & King County. “The federal announcement of five doses per vial was, I think, incredibly optimistic and what we’re seeing in real life is three to four doses per vial.”
Hannan, head of the Association of Immunization Managers, has heard the same concerns.
“Hopefully we will start to see more of the vials yielding five doses, but we’re not really seeing that consistently right now,” she says.
And yet it seems the federal government is assuming five doses per vial as it divvies up the supplies of vaccine and sends those out to health departments, says Del Becarro.
So far, much of the U.S. vaccine campaign has focused on reaching people who are unvaccinated and at increased risk of contracting monkeypox, but soon health departments will also have to be ready for the influx of people returning for their second doses 28 days later.
In the Seattle area, that could add up to about 4,000 people in the last week of August. And while it continues to be difficult to predict how the federal supply could change, Del Becarro says currently it looks like they will not be getting enough vaccine to do second shots while also providing first shots at a high rate.
The switch also requires new supplies and training, says Janna Kerins, medical director at the Chicago Department of Public Health. “It means using a different syringe, a different needle,” she says, “So it has taken a bit of time to make sure people have the supplies.”
Plus providers need technical training in how to administer a dose into the skin. And “we also need to educate [providers and the communities they serve] on the data that supports this change,” though there’s not much available, she says.
Distrust and feelings of disrespect
The new dosing strategy is also feeding into a strong sense of inequity among some in the communities most at risk for the disease.
The overwhelming majority of U.S. cases are still being detected among “men who reported recent sexual contact with other men,” CDC director Rochelle Walensky told reporters on Thursday.
Though the data is imperfect, what’s currently available shows another trend: a disproportionately high number of Black and LatinX members of the gay and queer community are getting monkeypox – and they’ve also had a hard time getting access to vaccines.
On Aug. 10, North Carolina’s health department released findings that 70% of the state’s cases have been detected in Black men, but just 24% of monkeypox vaccines have gone to this group.
Chicago is also seeing vaccination gaps in men of color. 30% of the city’s cases have been found among Latino men, but just 15% of vaccines have gone to the Latino population, according to Kerins, in Chicago. “We have some work to do to try to align the doses of vaccine better with those who are [at risk of] becoming cases,” she says.
National data indicates that queer Black and Brown communities are experiencing high rates of monkeypox: 33% of cases are occurring among those who are Hispanic and 28% among those who are Black.
While no national data has been shared on vaccinations, lack of access for these groups is a problem across the board, says Joseph Osmundson, a microbiologist at NYU and a queer community organizer in New York. The new dosing strategy could feed into that.
“We expect the data in New York and elsewhere to be similar,” Osmundson says. “What this [dosing strategy] is doing is using a different dosing regimen for those who get the vaccine late – who are more likely to be working class and more likely to be Black and Brown, who have not had the privilege, the ability to access vaccine yet.”
The disparities in vaccine access have sowed suspicion and distrust in communities of color, says Kenyon Farrow, with the advocacy group Prep4All.
Farrow says public health leaders still have to do more to explain why this new strategy is not necessarily inferior. He says a sentiment he’s seen online, especially from gay men of color, is that “they let White gay men take all the first full doses. And so we’re now supposed to believe that a fifth of that dose is going to do us just as well.”
Federal health officials say they’re working to bridge these disparities.
On Thursday, the White House monkeypox response team announced a pilot program to bring vaccines to Pride festivals and events where they can reach the gay, bisexual and queer communities at highest risk for contracting the virus.
“Many of the events we’re focusing on are events that focus on populations who are overrepresented in this outbreak,” including Black and Latino individuals, Dr. Demetre Daskalakis, deputy coordinator of the national monkeypox response, said on Thursday during a briefing with federal health officials.
“It’s really about positioning messaging and biomedical interventions where people can reach it, and also making sure that we’re going to the right places and talking about the right people.”
Copyright 2022 NPR. To see more, visit https://www.npr.org.
9(MDAxODM0MDY4MDEyMTY4NDA3MzI3YjkzMw004))
9(MDAxODM0MDY4MDEyMTY4NDA3MzI3YjkzMw004))









