Malcolm Reid recently marked the anniversary of his HIV diagnosis on Facebook. “Diagnosed with HIV 28 years ago, AND TODAY I THRIVE,” he wrote in a post in April, which garnered dozens of responses.
Reid, an advocate for people with HIV, said he’s happy he made it to age 66. But growing older has come with a host of health issues. He survived kidney cancer and currently juggles medications to treat HIV, high blood pressure, and Type 2 diabetes. “It’s a lot to manage,” he says.
But Reid’s not complaining. When he was diagnosed, HIV was sometimes a death sentence. “I’m just happy to be here,” Reid says. “You weren’t supposed to be here, and you’re here.”
More than half of the people living with HIV in the United States are, like Reid, 50 or older. Researchers estimate that 70% of people living with the virus will fall in that age range by 2030. Aging with HIV means an increased risk of other health problems, such as diabetes, depression, and heart disease, and a greater chance of developing these conditions at a younger age.
More than half a million people
Yet the U.S. health care system isn’t prepared to handle the needs of the more than half a million people — those already infected and those newly infected with HIV — who are older than 50, say HIV advocates, doctors, government officials, people living with HIV, and researchers.
They worry that funding constraints, an increasingly dysfunctional Congress, holes in the social safety net, untrained providers, and workforce shortages leave people aging with HIV vulnerable to poorer health, which could undermine the larger fight against the virus.
“I think we’re at a tipping point,” says Dr. Melanie Thompson, an Atlanta internal medicine physician who specializes in HIV care and prevention. “It would be very easy to lose the substantial amount of the progress we have made.”
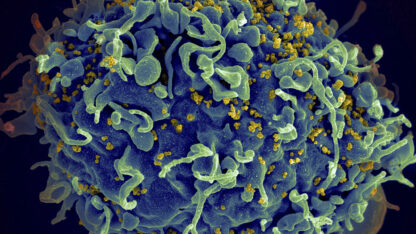
People are living longer with the virus due in part to the development of antiretroviral therapies — drugs that reduce the amount of virus in the body.
But aging with HIV comes with a greater risk of health problems related to inflammation from the virus and the long-term use of harsh medications. Older people often must coordinate care across specialists and are frequently on multiple prescriptions, increasing their risk for adverse drug reactions.
‘Dual stigma’
Some people face what researchers call the “dual stigma” of ageism and anti-HIV bias. They also have high rates of anxiety, depression, and substance use disorders.
Many have lost friends and family to the HIV/AIDS epidemic. Loneliness can increase the risks of cognitive decline and other medical conditions in older adults and can lead patients to stop treatment. It isn’t an easy problem to solve, says Dr. Heidi Crane, an HIV researcher and clinician at the University of Washington.
“If I had the ability to write a prescription for a friend — someone who’s supportive and engaged and willing to go walking with you twice a week — the care I provide would be so much better,” she says.
The complexity of care is a heavy lift for the Ryan White HIV/AIDS Program, the federal initiative for low-income people with HIV. The program serves more than half of the Americans living with the virus, and nearly half of its clients are 50 or older.
“Many of the people aging with HIV were pioneers in HIV treatment,” says Laura Cheever, who oversees the Ryan White program for the Health Resources and Services Administration, or HRSA. Researchers have a lot to learn about the best ways to meet the needs of the population, she said.
“We are learning as we go, we all are. But it certainly is challenging,” she says.
The Ryan White program’s core budget has remained mostly flat since 2013 despite adding 50,000 patients, Cheever says. The Biden administration’s latest budget request asks for less than half a percent bump in program funding.
Local and state public health officials make the bulk of the decisions about how to spend Ryan White money, Cheever says, and constrained resources can make it hard to balance priorities.
“When a lot of people aren’t getting care, how do you decide where that next dollar is spent?” Cheever says.
The latest infusion of funding for Ryan White, which has totaled $466 million since 2019, came as part of a federal initiative to end the HIV epidemic by 2030. But that program has come under fire from Republicans in Congress, who last year tried to defund it even though it was launched by the Trump administration.
It’s a sign of eroding bipartisan support for HIV services that puts people “in extreme jeopardy,” says Thompson, the Atlanta physician.
She worries that the increasing politicization of HIV could keep Congress from appropriating money for a pilot student loan repayment program for health professionals that aims to lure infectious disease doctors to areas that have a shortage of providers.
Many people aging with HIV are covered by Medicare, the public insurance program for people 65 and older. Research has shown that Ryan White patients on private insurance had better health than those on Medicare, which researchers linked to better access to non-HIV preventive care.
Some 40% of people living with HIV rely on Medicaid, the state-federal health insurance program for low-income people. The decision by 10 states not to expand Medicaid can leave older people with HIV few places to seek care outside of Ryan White clinics, Thompson says.
“The stakes are high,” she says. “We are in a very dangerous place if we don’t pay more attention to our care systems.”
About 1 in 6 new diagnoses are in people 50 or older but public health policies haven’t caught up to that reality, says Reid, the HIV advocate from Atlanta. The Centers for Disease Control and Prevention, for instance, recommends HIV testing only for people ages 13 to 64.
“Our systems are antiquated. They, for some reason, believe that once you hit a certain number, you stop having sex,” Reid says. Such blind spots mean older people often are diagnosed only after the virus has destroyed the cells that help the body fight infection.
Funds to improve
In acknowledgment of these challenges, HRSA recently launched a $13 million, three-year program to look at ways to improve health outcomes for older people living with HIV.
Ten Ryan White clinics across the United States participate in the effort, which is testing ways to better track the risk of adverse drug interactions for people taking multiple prescriptions. The program is also testing ways to better screen for conditions like dementia and frailty, and ways to streamline the referral process for people who might need specialty care.
New strategies can’t come quickly enough, says Jules Levin, executive director of the National AIDS Treatment Advocacy Project, who, at age 74, has been living with HIV since the 1980s.
His group was one signatory to “The Glasgow Manifesto,” in which an international coalition of older people with HIV called on policymakers to ensure better access to affordable care, to enablepatients to get more time with doctors, and to fight ageism.
“It’s tragic and shameful that elderly people with HIV have to go through what they’re going through without getting the proper attention that they deserve,” Levin says. “This will be a disaster soon without a solution.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF — the independent source for health policy research, polling, and journalism.