The target group is people who have visited the ER at least six times over a six-month period. Many are poor and without jobs, and some are homeless. A high percentage have no health insurance.
Many of these people abuse drugs or have untreated mental illness. They also tend to have chronic diseases such as diabetes and hypertension.
Atlanta’s main safety-net hospital, Grady Memorial, is running a program that helps these ER ‘’frequent flyers’’ better manage their health through primary care – and not in an emergency room, which is the most expensive place to get medical services.
From Grady’s standpoint, its Chronic Care Clinic aims to reduce unnecessary use of its emergency services while connecting patients to the medical and social services they need.
The first results are promising, Grady officials say.
Shannon Sale, Grady Health System’s chief strategy officer, says the health system “had concern about cases that could be seen in primary care settings’’ – such as for prescription refills and ongoing care for chronic conditions – but kept showing up in ERs.
The program may serve as a pilot project for the Grady “waiver’’ proposal that aims to provide health coverage for potentially thousands of people who currently have no insurance.
“We’re using it as a proof of concept or a test run for what would be possible under a waiver program,’’ says Matt Hicks, a Grady vice president.
Frequent use of the ER is not just an Atlanta problem. An Annals of Emergency Medicine study in 2010 reported that frequent users make up between 4.5 percent and 8 percent of all emergency patients and are responsible for 21 percent to 28 percent of all emergency department visits.
The president of the American College of Emergency Physicians says some health systems such as Grady are trying to provide places for these patients to get routine maintenance care.
“Emergency physicians welcome this,’’ says Dr. Vidor Friedman, who practices in Orlando. “We’re all trying to do the right thing for patients and get them to the appropriate site of care.”
A Washington state program, he notes, helped save its Medicaid program “a great deal of money’’ by steering these patients into primary care.
But he also adds that many patients who wind up in the ER frequently are fragile medically or psychologically.
Still, Jimmy Lewis of HomeTown Health, an association of rural hospitals in Georgia, says some of these facilities have managed to reduce unnecessary ER use through programs such as “home visits,’’ in which EMS crews act as case managers for patients in their homes.
These visits, Lewis says, can help keep some recently discharged patients from being readmitted to the hospital. That’s important for financially struggling rural facilities because too many readmissions of a hospital’s Medicare patients can cause a cut in federal payments.
Many of the frequent ER users in rural areas have mental health needs, Lewis adds.
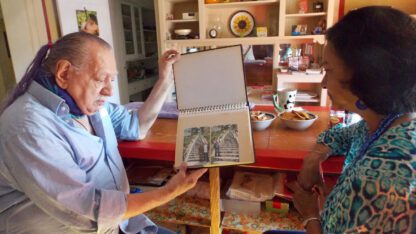
The Grady Chronic Care Clinic identifies frequent ER users, then connects them with a care team that has physician oversight. The team consists of an advanced practice provider, clinical pharmacist, behavioral health specialist, community health worker, navigator and mobile integrated health provider.
“We engage them in their first ED visit and give them a care plan,’’ says Sale of Grady.
The patients are educated in the appropriate use of the emergency department, says Karen Sutton, senior licensed mental health clinician for the Grady program. “We want to help them graduate to long-term primary care.”
“We’re seeing that at least 35 percent to 40 percent are doing a great job of maintaining appointments and consistency of taking medications,’’ Sutton says.
“We do have some who are very medically complex,’’ Sutton says. “We’re working on achieving a behavior change.’’
For some disadvantaged people, getting medical care is only one of several problems, and the Grady program addresses that. Community health workers can help them get an ID, apply for housing or apply for a job.
Some patients drop out of the program.
“They have so much instability” in their lives, Sutton says. “A lot of our patients remain homeless. With a lot of patients, we may be the only support they have.’’
Some come to the ER at night, she adds, because they “have nowhere else to go.’’
Grady partnered with United Way to open four beds for Chronic Care patients who are homeless.
“For patients we’ve been able to provide housing, it’s made a big difference,’’ Sutton says.
Chronic Care has up to 750 or more patients on its registry; the program will serve about 200 annually.
“It’s resource-intensive,’’ says Sale.
Kaiser Permanente has helped fund the Chronic Care Clinic. St. Jude’s Recovery Center helps supply addiction treatment.
Most of the Grady patients go through the program for three to six months, while some stay for up to a year. If necessary, patients can continue to receive help after their “graduation” from the program.
“We’ve seen better-than-expected results,’’ says Leslie Marshburn, director of Population Health at Grady. She says the program has led to a reduction in ER visits of close to 50 percent, and a similar decrease in total costs to the system for this group of patients.
The Grady waiver proposal would be broader than the ER patient program. It would use federal matching Medicaid dollars to help set up pilot sites that would give coverage to the uninsured, then manage their care and potentially improve their health. A waiver program would require federal approval. Grady’s Hicks points out that a waiver would replace foundation grants with government funding.
Brian Kemp, who will take office as Georgia governor on Jan. 14, is said to be favorable to such waiver ideas.
Kemp has Dr. Tom Price, a former U.S. secretary of health and human services, on his transition team. That choice could pave the way for a waiver plan, Kyle Wingfield of the Georgia Public Policy Foundation, told GHN recently.
Wingfield said a waiver would give Georgia the flexibility to design a pilot program as Grady envisions and see how it works. The goal would be “to find a better way to spend the money″ from the feds, he said.
Andy Miller is editor and CEO of Georgia Health News