If you’re just getting sick with COVID-19, and you’re at high risk for severe disease, there are two kinds of pills – scattered across pharmacies in the U.S. – that could help prevent you from getting worse. But doctors say the two pills are not equal.
These antiviral pills – molnupiravir from Merck and Paxlovid from Pfizer – help stop the virus from spreading throughout the body when taken early in the course of illness. Both were authorized by the FDA towards the end of December, and are distributed by the U.S. government.
But molnupiravir is a much less effective drug, and many doctors have been reluctant to prescribe it. “It’s an alternative rather than a first-line drug, and I think that’s why the utilization is lower,” says Dr. Rajesh Gandhi, of Mass General Hospital in Boston, who helps develop COVID-19 treatment guidelines for the NIH and the IDSA, a medical society.
Both antivirals are five-day pill courses that can only be prescribed to someone who’s tested positive for COVID, and must be started within five days of getting symptoms.
Data reviewed by the FDA showed molnupiravir was just 30% effective at cutting the risk of getting hospitalized with COVID-19. Paxlovid works much better, reducing the same risk by nearly 90%. Antibody and antiviral infusion treatments also reduce the risk of severe disease more than molnupiravir, according to published data. And molnupiravir comes with reproductive risks, so it’s not generally recommended for patients who are pregnant or trying to conceive.
On the shortlist of four early COVID-19 treatments recommended by the government for patients before they need hospitalization, molnupiravir comes last – for use only when the other treatments can’t be used.
The federal government spent $2.2 billion on molnupiravir – and many doses are sitting unused. Some pharmacies “are running into issues with storage space on molnupiravir and not moving the product that quickly,” Dr. Derek Eisnor, who leads the government’s distribution of COVID drugs, said on a call with state health officials recently.
Still, the other, more effective drugs have their drawbacks too. Paxlovid pills have a long list of common drugs you can’t take with them because of possibly dangerous interactions. Getting intravenous drug infusions – as patients do for the other two authorized treatments – requires going into a clinic, sometimes multiple times. And many of these treatments are in short supply.
So Gandhi says there’s still a place for molnupiravir in the current COVID treatment landscape: as “an alternative when one of those other drugs can’t be given, because of drug interactions or feasibility issues.”
Trillium Health, a community health center in Rochester, N.Y., treats “a lot of complicated patients, who have complex med lists, whose drugs cannot always be discontinued,” says Dr. Bill Valenti, co-founder and staff physician.
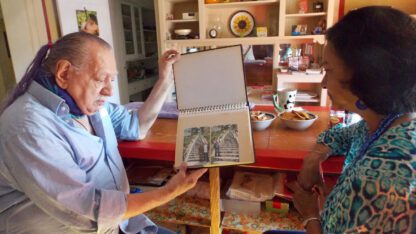
The health center has found a use for molnupiravir, prescribing it to more than a dozen patients, including Valenti’s 55-year-old patient John DeGrandis. “I’m kind of his guinea pig sometimes,” DeGrandis jokes.
The first time DeGrandis got COVID, it was in fall 2020, before vaccines and treatments were available — and it felt like a really bad cold.
This month, when he got it again, there were authorized drugs for treating mild COVID. “I think it’s preferable to treat than not to treat,” Valenti says, “So we went through the list.”
At the top of the list was Paxlovid — but Valenti ruled it out because it might have some bad interactions with other medications DeGrandis was taking.
Then there was a long waiting list for infusions, which could take a while to get. “That really wasn’t an option,” Valenti says, since the point of early COVID treatments is to stop the virus from spreading throughout the body.
That left molnupiravir – which was plentiful at the local pharmacy, and easy to take at home. While it is not as effective as the other options, “maybe we can balance that out by giving it to him early in the course of his illness,” Valenti reasoned.
So DeGrandis filled his prescription at Walgreens, and took four pills, twice a day, for five days. At the end of the course, did it help? Unclear, says DeGrandis: “I don’t know the difference. I honestly have not felt bad the whole time. I was a little tired, but now I feel 100%.”
Valenti says these COVID pills are the first generation of tools doctors can use to treat COVID patients early. “These drugs are good for the time, especially since it took so little time to find something that was helpful. But I think this is just the beginning of the treatment era,” he says.
Better drugs that take fewer pills and are more effective are under development. For now, he’ll work with what he’s got.
Copyright 2022 NPR. To see more, visit https://www.npr.org.
9(MDAxODM0MDY4MDEyMTY4NDA3MzI3YjkzMw004))

9(MDAxODM0MDY4MDEyMTY4NDA3MzI3YjkzMw004))