Almost 3 million people in Georgia rely on Medicaid health insurance, including thousands of people who signed up earlier in the COVID-19 pandemic.
Now, federal pandemic rules are changing and millions of people nationwide are losing — or are about to lose — their health coverage over the next year.
Georgia has already cut tens of thousands of adults and children from the safety net program for low-income people and people with certain disabilities.
This fall, Marrow Woods is excited to be a junior in college.
“Which is very surprising. I had a surgery last December and I had to leave school early and go on a medical leave,” Woods said, “so, I’m just happy that I was able to do that and stay on track for school.”
Woods has an inflammatory condition called Hidradenitis Suppurativa that attacks the body’s hair follicles. It’s painful and can be debilitating.
The 20-year-old Macon student, who uses they and them pronouns, has to travel to Atlanta every few weeks for medical treatment.
“I go to the cancer center to get them because that’s the only place where they administer the medication,” Woods said.
The specialized treatment, called an infusion, is expensive. It’s much more than their family can afford.
Woods said they’re grateful Medicaid makes the treatment attainable. It’s helping.
“The infusion and my ability to be on it because I am on Medicaid,” Woods said, “this has really been something that has allowed me to manage my chronic illness in a way that I wasn’t able to before.”
But that progress could be at risk.
Until this spring, federal COVID-19 public health emergency rules prohibited states from removing anyone from Medicaid.
Now, states are reevaluating everyone in the low-income health insurance program to check if they still financially qualify for it.
The United States Department of Health and Human Services expects around 7 million people to lose Medicaid even though they are still eligible for the coverage, at least temporarily.
Woods said they’re worried they could lose coverage in the redetermination process and no longer be able to access the critical infusion treatments or finish school on time.
“It would be devastating,” they said.
States across the country have cut almost four-million people from the safety net program so far, according to a KFF News analysis.
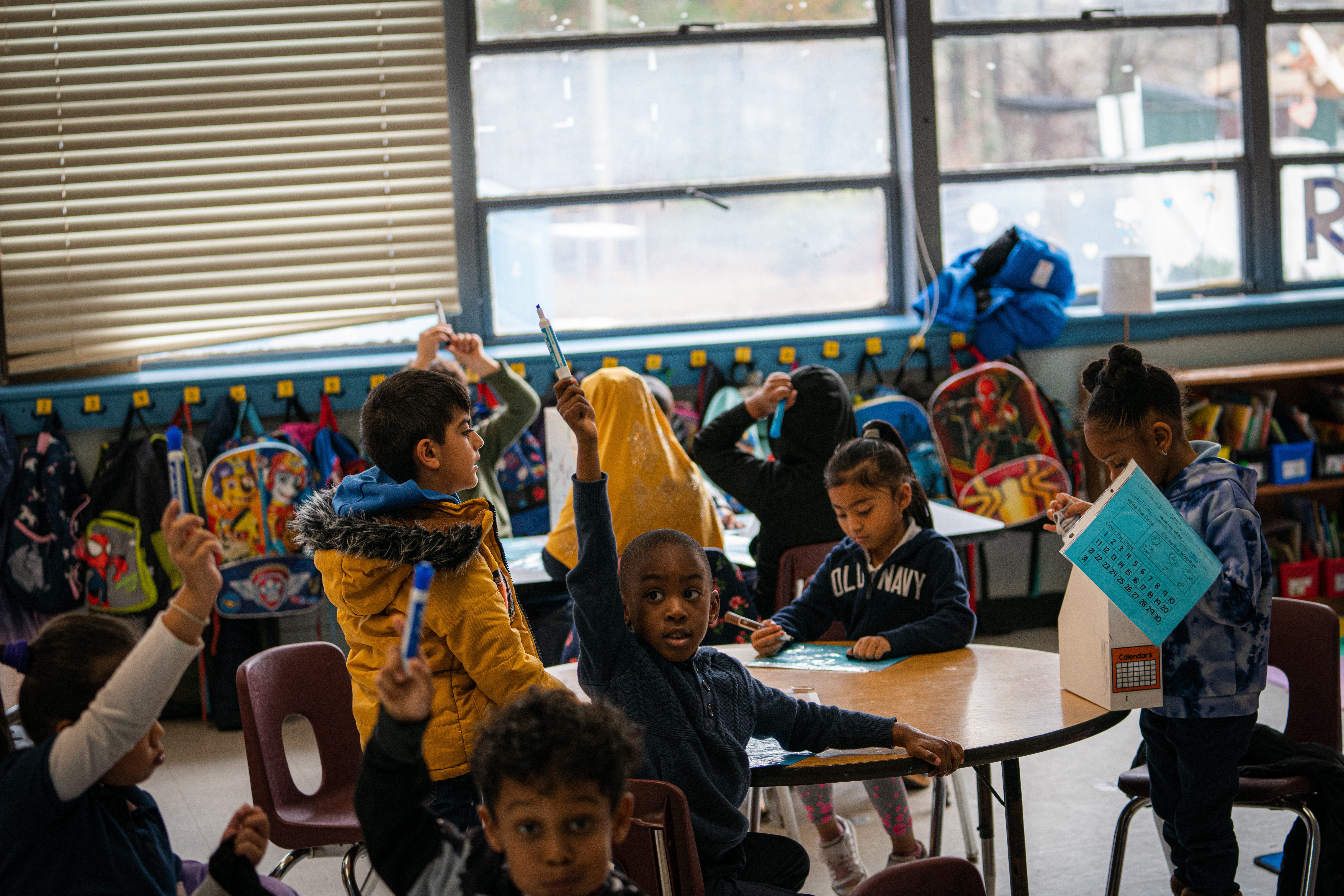
Georgia has so far removed around 100,000 people, including children on PeachCare for Kids.
The numbers make Georgia a top-five state for Medicaid terminations.
“Children are going to be the main ones losing coverage in Georgia,” said research professor Joan Alker, also the executive director of the Center for Children and Families at the Georgetown McCourt School of Public Policy.
She said too many low-income families are losing Medicaid coverage for “procedural” reasons.
Like not completing renewal paperwork, an incorrect mailing address or a typo.
Basically: red tape.
And many low-income families who lose Medicaid won’t be able to afford to buy other insurance, she said, especially in the ten states, including Georgia, that haven’t expanded Medicaid under the Affordable Care Act.
“A lot of parents are going to fall into the coverage gap,” Alker said. “Georgia is a state where, during the pandemic when Medicaid could not be taken away from people, Georgia was one of the states where most of the enrollment growth was children and their parents and new mothers.“
Procedural Medicaid redetermination terminations would leave tens of thousands of people across the state with no coverage at all, health advocates fear, or leave them uncovered for a time before they find other options.
Madeline Ryan Smith is a disability advocate in Statesboro.
“It’s almost like we’re on this giant bus and we’re all in the bus driving full speed towards the edge of a cliff,” said Smith, who is running for a state House seat as a Democrat against Republican Swainsboro Representative Butch Parrish.
She said despite Georgia’s monthslong marketing campaign to get the word out about Medicaid recertification, a lot of people have no idea it’s even happening.
“Especially when we talk about the demographics of people who are already on Medicaid, Smith said, “that is, individuals who are low income, working more than one low-wage job, where they don’t have time to listen to the news on a daily basis, to read that newsletter in their inbox about their Medicaid status.”
Smith, who’s blind, said people with disabilities face additional hurdles in meeting Medicaid renewal deadlines.
“They might be living in an area where they don’t have access to internet, public transportation,” she said, “or they might not even be able to get to their mailbox physically.”
Georgia officials have stressed that everyone on Medicaid and PeachCare for Kids gets a series of renewal notices, calls or text messages leading up to their individual deadlines.
And anyone found ineligible to renew their health insurance can appeal the termination.
Woods is still waiting for a renewal date.
The uncertainty is a reminder of what could happen if they lose Medicaid and their medical treatment is interrupted.
“The lowest point of me dealing with this chronic illness was when I was bedridden for a few months, I mean, completely dependent on my mother,” Woods said.
Woods still must use a cane to get around campus. They struggle with muscle weakness and other symptoms.
And with almost another year of national Medicaid redetermination to go, the Biden administration is urging all state governors to do more to ensure people who do qualify for Medicaid coverage don’t inadvertently lose it.
Health advocates are hoping that’s enough.