Health Reform To Cost Georgia Extra $128 Million Over Next Two Years
Georgia health officials anticipate spending an additional $128 million over the next two years as a result of the federal health reform law.
The board of Georgia’s Department of Community Health Thursday signed off on budget plans for the 2014 and 2015 fiscal years. They included the Affordable Care Act’s estimated financial impact.
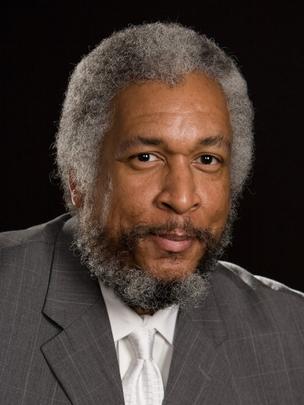
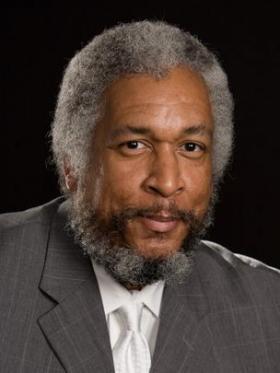
Board Chairman Norman Boyd wasn’t pleased.
“Here’s a $100 million being taken out of the taxpayers’ pocket of Georgia. I think that’s a significant amount of money and not sure what we’re getting in return for that,” said Boyd.
Since the state has rejected the law’s optional Medicaid expansion, much of the added costs are associated with two other elements of the rollout.
The first element is the review period for Georgia’s 1.8 million Medicaid and Peachcare for Kids enrollees will be extended from every six months to every 12 months.
“When we did a six month review, we might have uncovered people who would not be eligible and we’d take them off the roll and there’d be a savings associated with that,” said DCH commissioner Clyde Reese, who opposes the change. “If we do a 12 month review, then we’re not going to catch those people at six months. We’ll only catch them at the end of the year so for six months we’ll incur additional costs.”
But Amanda Ptashkin of the nonprofit Georgians For A Healthy Future argues the extended review period will ultimately improve patient care.
“Folks can either miss a notification or miss a phone call or something and easily fall of the roles and that impacts their care directly. Prevents them from seeing a doctor, from getting a prescription that’s necessary to fill and their health suffers the consequences from that.”
The second element factored into the state’s estimated cost is based on what is known in policy circles as the “woodwork effect.” Some people currently qualify for assistance but aren’t enrolled because they don’t know they’re eligible. Those people, state officials say, are expected to ‘come out of the woodwork’ and sign up for coverage.
State officials estimate more than 60,000 low-income kids will gain insurance over the next two years simply because their parents have new ways to find out if they’re eligible for existing programs.
“I think it is a good thing that people start hearing about their options and if that means that people are eligible for Medicaid in our current system then that’s great. With 1.9 million uninsured, having people have greater access to coverage is a good thing,” said Ptashkin.
A state health exchange, which will be web-based and online in October, is one of the new ways people will find out if their eligible for assistance.
9(MDAxODM0MDY4MDEyMTY4NDA3MzI3YjkzMw004))




