An unheard alarm
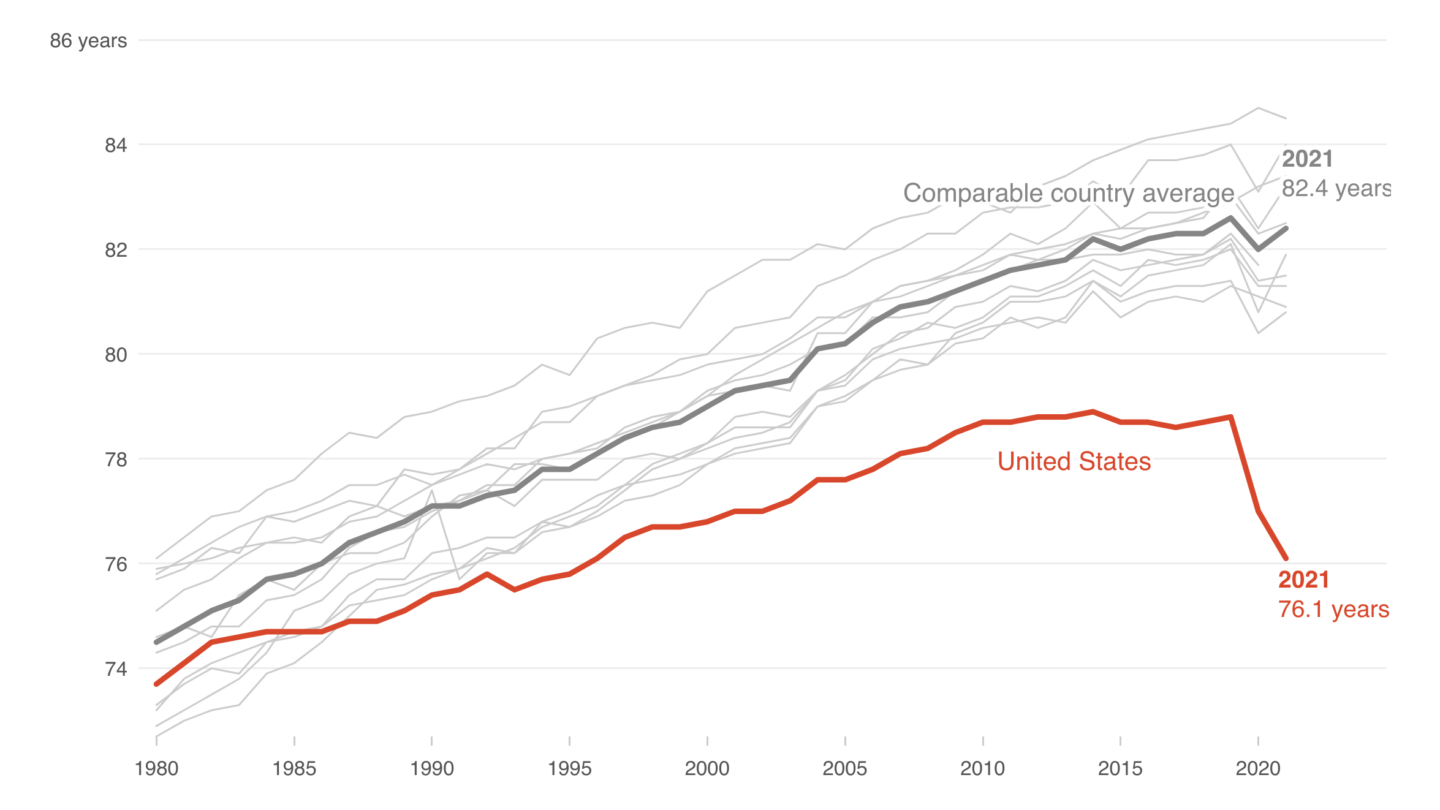
One group of people are not surprised at all: Woolf and the other researchers involved in a landmark, 400-page study ten years ago with a name that says it all: “Shorter Lives, Poorer Health.” The research by a panel convened by the National Academy of Sciences and funded by the National Institutes of Health compared U.S. health and death with other developed countries. The results showed – convincingly – that the U.S. was stalling on health advances in the population while other countries raced ahead.
The authors tried to sound an alarm, but found few in the public or government or private sectors were willing to listen. In the years since, the trends have worsened. American life expectancy is lower than that of Cuba, Lebanon, and Chechnya.
Ten years later, here’s a look back at what that eye-popping study found, and why the researchers involved believe it’s not too late to turn the trends around.
Beyond bad habits
Americans are used to hearing about how their poor diets and sedentary lifestyles make their health bad. It can seem easy to brush that off as another scold about eating more vegetables and getting more exercise. But the picture painted in the “Shorter Lives” report could shock even those who feel like they know the story.
“American children are less likely to live to age 5 than children in other high-income countries,” the authors write on the second page. It goes on: “Even Americans with healthy behaviors, for example, those who are not obese or do not smoke, appear to have higher disease rates than their peers in other countries.”
The researchers catalog what they call the “U.S. health disadvantage” – the fact that living in America is worse for your health and makes you more likely to die younger than if you lived in another rich country like the U.K., Switzerland or Japan.
“We went into this with an open mind as to why it is that the U.S. had a shorter life expectancy than people in other countries,” says Woolf, who chaired the committee that produced the report. After looking across different age and racial and economic and geographic groups, he says, “what we found was that this problem existed in almost every category we looked at.”
That’s why, says Eileen Crimmins, professor of gerontology at the University of Southern California who was also on the panel that produced the report, they made a deliberate choice to focus on the health of the U.S. population as a whole.
“That was a decision – not to emphasize the differences in our population, because there is data that actually shows that even the top proportion of the U.S. population does worse than the top proportion of other populations,” she explains. “We were trying to just say – look, this is an American problem.”
Digging into the ‘why’
The researchers were charged with documenting how Americans have more diseases and die younger and to explore the reasons why.
“We were very systematic and thorough about how we thought about this,” says Woolf. The panel looked at American life and death in terms of the public health and medical care system, individual behaviors like diet and tobacco use, social factors like poverty and inequality, the physical environment, and public policies and values. “In every one of those five buckets, we found problems that distinguish the United States from other countries.”
Yes, Americans eat more calories and lack universal access to health care. But there’s also higher child poverty, racial segregation, social isolation, and more. Even the way cities are designed makes access to good food more difficult.
“Everybody has a pet thing they worry about and say, ‘it’s oral health’ or ‘it’s suicides’ – everyone has something that they’re legitimately interested in and want to see more attention to,” says John Haaga, who was the director of the Division of Behavioral and Social Research at the National Institute on Aging at NIH, before he retired. “The great value of an exercise like this one was to step back and say, ‘OK, all of these things are going on, but which of them best account for these long-term population level trends that we’re seeing?’ “
The answer is varied. A big part of the difference between life and death in the U.S. and its peer countries is people dying or being killed before age 50. The “Shorter Lives” report specifically points to factors like teen pregnancy, drug overdoses, HIV, fatal car crashes, injuries, and violence.
“Two years difference in life expectancy probably comes from the fact that firearms are so available in the United States,” Crimmins says. “There’s the opioid epidemic, which is clearly ours – that was our drug companies and other countries didn’t have that because those drugs were more controlled. Some of the difference comes from the fact that we are more likely to drive more miles. We have more cars,” and ultimately, more fatal crashes.
“When we were doing it, we were joking we should call it ‘Live free and die,’ based on the New Hampshire slogan, [‘Live free or die’],” Crimmins says. “The National Academy of Sciences said, ‘That’s outrageous, that’s too provocative.’ “
There are some things Americans get right, according to the “Shorter Lives” report: “The United States has higher survival after age 75 than do peer countries, and it has higher rates of cancer screening and survival, better control of blood pressure and cholesterol levels, lower stroke mortality, lower rates of current smoking, and higher average household income.” But those achievements, it’s clear, aren’t enough to offset the other problems that befall many Americans at younger ages.
All of this costs the country tremendously. Not only do families lose loved ones too soon, but having a sicker population costs the country hundreds of billions of dollars every year in extra health care costs.
“Behind the statistics detailed in this report are the faces of young people – infants, children, and adolescents – who are unwell and dying early because conditions in this country are not as favorable as those in other countries,” the paper’s authors wrote.
Little action, despite the stakes
“Shorter Lives” is filled with recommended next steps for the government, especially the NIH, which has a budget of more than $40 billion annually to conduct research to improve Americans’ health.
The NIH should undertake a “thorough examination of the policies and approaches that countries with better health outcomes have found useful and that may have application, with adaptations, in the United States,” the authors wrote.
In other words: let’s figure out what they are doing that works in other places, and do it over here.
Dr. Ravi Sawhney, who helped conceive of and launch the “Shorter Lives” study at NIH before he says he was “driven out” of the agency, had high hopes that the report would make a mark. “I really thought that when the results came out, they would be so obvious that people would say: Let’s finally do this,” he says.
Ten years on, how much of the detailed action plan has been done?
“To be brief, very little of that happened,” Woolf says. At the time, he says, NIH officials didn’t seem very interested in raising awareness about the panel’s findings or in following up on its proposed research agenda. “There was some media coverage at the time that the report rolled out, but NIH was not involved in trying to promote awareness about the report.”
Crimmins agrees. “There was a little bit more research, but there wasn’t any policy reaction,” she says. “I thought there might be, because it’s embarrassing, but it just tends to be ignored.” Those who are interested in this issue, she notes, tend to be those invested in “marvelous things they think are going to delay aging,” even though people older than 75 are the only age group in the country that already does comparatively well.
Haaga, the former NIH division director, also thinks the response at the agency was lacking. “Not nearly enough has been done, given the stakes and given what we could learn,” he says.
In response to NPR’s request for comment for this story, NIH pointed to a subsequent panel on midlife mortality, several initiatives the agency has undertaken on disparities between subgroups within the U.S., and a recent paper funded by NIH that looked again at international life expectancy.
Outgoing NIH Director Francis Collins told NPR in 2021 that it bothered him that there hadn’t been more gains to American life expectancy during his tenure. In his view, the success of NIH in achieving scientific breakthroughs hadn’t translated to more gains because of problems in society that the research agency had little power to change.
Woolf calls it a misconception to assume that America’s great scientific minds and medical discoveries translate to progress for the health of the population. “We are actually very innovative in making these kinds of breakthroughs, but we do very poorly in providing them to our population,” he says.
‘We can’t touch everything’
Department of Health and Human Services Secretary Xavier Becerra answered NPR’s question at a press conference earlier this month about work the agency was doing to address lagging life expectancy by mentioning COVID-19 and vaccine hesitancy, along with mental health issues and gun violence.
“There’s so many things that we’re doing,” Becerra said. “We can’t touch everything. We can’t touch state laws that allow an individual to buy an assault weapon and then kill so many people. We can only come in afterwards.”
CDC Director Rochelle Walensky responded by listing some of the agency’s work on mental health and vaccines, and acting NIH director Larry Tabak pointed to research on health disparities.
HHS did not answer a follow up question about whether the agency has considered a national commission or similar effort to address American life expectancy and poor health.
Sawhney thinks the federal government should try harder to fix the problems documented in the “Shorter Lives” report. He doesn’t think lack of public awareness is the problem. “I really think that most Americans know that Americans are more overweight and obese and that we have higher rates of disease and live shorter lives than other countries,” he says, “It’s just the NIH and the CDC that don’t want to take the responsibility for that failure or to do anything about it.”
Crimmins says, in her experience, lawmakers and federal health officials don’t like talking about how the U.S. is lagging behind other countries.
“I convened a meeting in Washington with the National Center for Health Statistics [part of CDC] about increasing healthy life expectancy,” she recalls. “It was a relatively small meeting, but we brought experts from Canada.” An official at the time gave what she calls a “typical” response, saying: “Oh, we can’t have anything but an American solution to these issues – we can’t listen to other countries.”
“International studies are not the flavor of the month – they never will be,” says Haaga. “The problem with foreign countries is that they’re not in someone’s congressional district.”
It’s more than a missed opportunity, says Woolf. It’s a tragedy.
“If you add up the excess deaths that have occurred in the United States because of this unfolding problem, it dwarfs what happened during COVID-19, as horrible as COVID-19 was,” Woolf says. “We’ve lost many more Americans cumulatively because of this longer systemic issue. And if the systemic issue is unaddressed, it will continue to claim lives going forward.”
Small victories are possible
Taking stock of the many ways in which Americans are sicker and die younger can be overwhelming, says Haaga. “It’s such a long list, that might partly be why the issue doesn’t grab people,” he says. “They just go, ‘Oh, my gosh, that’s depressing, what’s on the other channel?’ But there’s a lot of things that could be done, and small victories are victories.”
According to the “Shorter Lives” report, “the important point about the U.S. health disadvantage is not that the United States is losing a competition with other countries, but that Americans are dying and suffering at rates that are demonstrably unnecessary.”
Rather than feel overwhelmed at the immensity of the problems, Sawhney suggests, the focus should instead be on the fact that every other rich country has been able to figure out how to help people live longer, healthier lives. That means that Americans could do it too, he says.
He believes that the changes might not be as hard as some policymakers and health officials seem to think. “You look at these healthier countries, they’re free countries – England, France, Italy – they’re not banning delicious foods. They’re not chaining people to treadmills,” he says. “Americans love to travel to Europe, to Australia, to Canada to enjoy their foods and their lifestyles, and so the idea that we might say, ‘Hey, maybe we could bring some of those lifestyles back’ – I don’t think people are going to go up in arms that we’re taking away their freedoms.”
Getting policy ideas from other countries is just an obvious move, Woolf adds. “If a martian came down to earth and saw this situation, it would be very intuitive that you [would] look at other countries that have been able to solve this problem and apply the lessons learned,” he says.
In historical research he’s been doing, “I found that there are dozens and dozens of countries on almost every continent of the world that have outperformed the United States for 50 years,” he says. “It’s worth taking a look at what they’ve done and Americanizing it – you don’t have to take it right off the shelf.”
Some of the policies he’s identified as helpful include universal, better coordinated health care, strong health and safety protections, broad access to education, and more investments to help kids get off to a healthy start. These policies are “paying off for them,” he says, and could for Americans, too.
Copyright 2023 NPR. To see more, visit https://www.npr.org.
9(MDAxODM0MDY4MDEyMTY4NDA3MzI3YjkzMw004))
9(MDAxODM0MDY4MDEyMTY4NDA3MzI3YjkzMw004))