In late November, more than 110 people gathered at a crowded Christmas party at a restaurant in Oslo. Most of the guests were fully vaccinated. One had returned from South Africa just a few days earlier and was unknowingly carrying the omicron variant of SARS-CoV-2.
Ultimately, about 70% of the partygoers were infected.
Scientists who traced this super spreader event concluded it was evidence that omicron was “highly transmissible” among fully-vaccinated adults.
Just over a month later, omicron’s speedy worldwide ascent now makes it abundantly clear that the party wasn’t an isolated example. In country after country, the new variant has outcompeted its predecessor, the delta variant — with one case of omicron sparking at least three other new infections on average. Cases have soared to record highs in parts of Europe and now the U.S., where about half a million new infections have been recorded in a single day.
“This is a game-changing virus, especially in the vaccinated population where people have had a level of invincibility,” says Sumit Chanda, a professor in the Department of Immunology and Microbiology at Scripps Research.
Indeed, in a world where vaccinations and infections have built up immunity, other variants were having trouble gaining a foothold. Yet omicron is thriving.
“This changes the calculus for everybody,” says Chanda.
And so scientists are trying to figure out: What accounts for omicron’s lightning quick spread?
While it’s still early, they’re starting to piece together why the new variant is so contagious — and whether that means old assumptions about how to stay safe need to be revamped.
A big question: How does it fare in the air?
So far, omicron’s best trick — what helps explain its success more than anything else — is dodging our immunity: the antibodies and other immune defenses put on by the body after vaccination and/or prior infection.
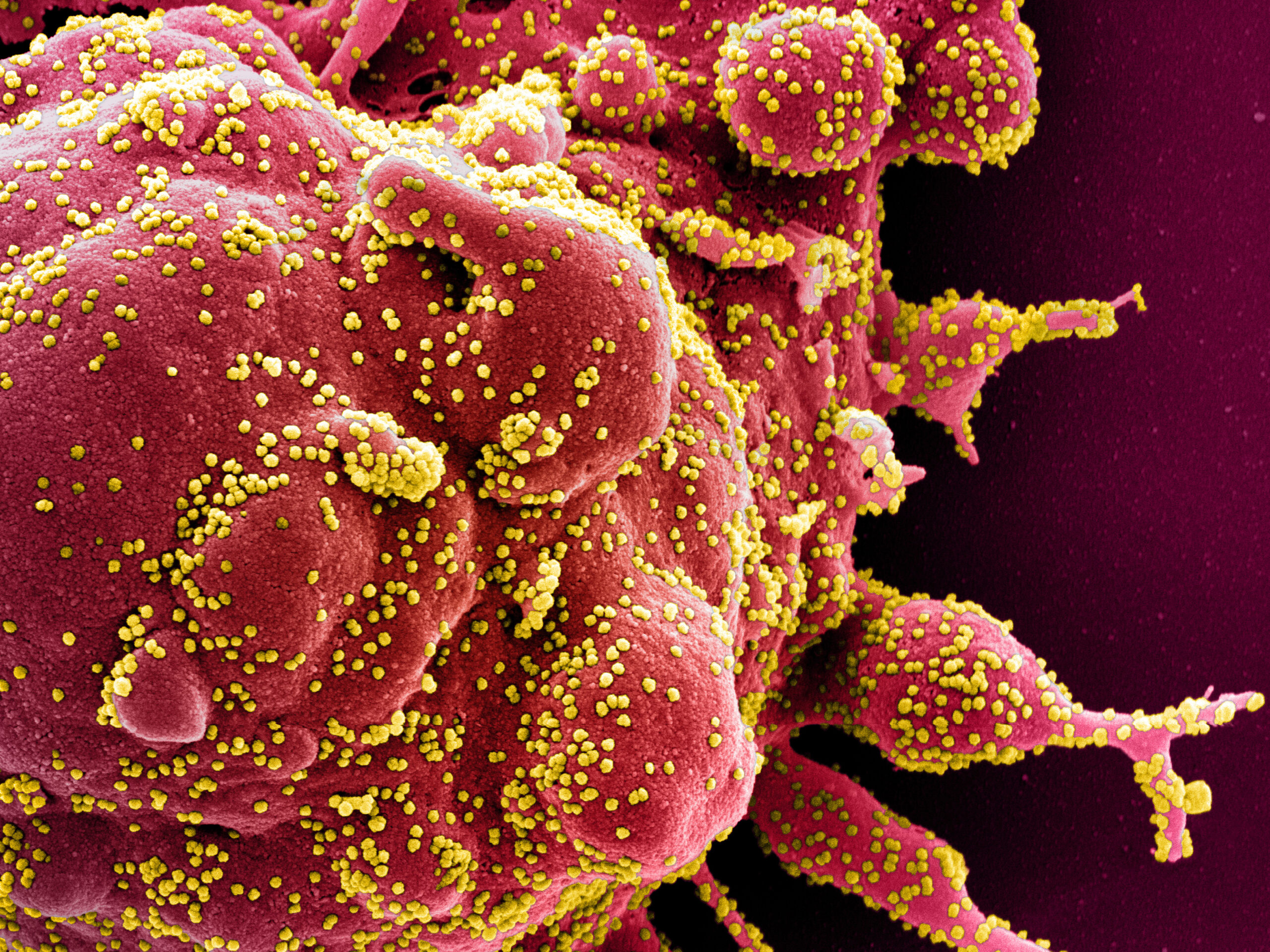
The variant’s many mutations on the spike protein allow it to infect human cells more efficiently than previous variants could, leaving many more people again vulnerable. Because of that, “immune escape” alone could be the major reason why the variant looks so contagious compared to delta, which was already highly transmissible.
In fact, omicron has been spreading at a pace that’s comparable to how fast the original strain of the coronavirus spread at the very beginning of the pandemic despite the world’s newfound levels of immunity.
“The playing field for the virus right now is quite different than it was in the early days,” says Dr. Joshua Schiffer, an infectious disease researcher at Fred Hutchinson Cancer Research Center. “The majority of variants we’ve seen to date couldn’t survive in this immune environment.” Even delta was essentially at a “tie,” he says, where it was persisting, but “not growing very rapidly or decreasing very rapidly.”
A new study from Denmark suggests that much of the variant’s dominance comes down to its ability to evade the body’s immune defenses.
Researchers compared the spread of omicron and delta among members of the same household and concluded that omicron is about 2.7 to 3.7 times more infectious than the delta variant among vaccinated and boosted individuals.
But here’s an interesting additional point: For unvaccinated people, there was no significant difference in rates of infection between delta and omicron. That would indicate that both variants are about at the same level of transmissibility among the unvaccinated — in other words, under those circumstances, omicron is not necessarily more transmissible than delta.
If confirmed, the findings would support the idea that omicron’s increased transmissibility can be ascribed to its “immune evasiveness” — not some other characteristics that make the variant inherently more transmissible, the authors conclude.
This is also what a small study from the University of Maryland may hint at, although here, too, the findings are preliminary and yet to be peer reviewed.
Researchers measured how much virus vaccinated people who were infected with omicron were releasing into the air after shouting and singing. Four out of the five were exhaling ample amounts of virus into the air – comparable to the amount shed by unvaccinated people earlier in the pandemic.
“But what’s striking is that I was expecting to see the amounts be much higher, and they are not,” says Dr. Don Milton, an infectious disease aerobiologist at the University of Maryland School of Public Health, who led the study.
The findings suggest the spread of omicron could, in part, hinge on the fact that more vaccinated people are contagious and shedding virus, not necessarily that each infected individual is releasing a lot more virus into the air. And if the results hold true, Milton says long distance transmission is unlikely to become a new concern with omicron, above and beyond what’s already been seen with other contagious variants like delta.
“With measles, for example, the source strength is just so intense that even in the next room, people are still at risk of getting infected,” he says. “And you don’t see much of that with this virus” because it gets so diluted by the time it reaches the next room.
But there is a down side. Says Milton: “The bad news is the vaccine doesn’t mean you’re not going to transmit it to somebody else.”
And he adds that the findings are ultimately limited to those who are vaccinated: “Maybe you get an unvaccinated person, it [the amount of virus] is a whole lot more intense.”
Omicron could have other advantages that give it a leg up
With so many mutations, it’s still quite possible that omicron does have additional advantages that make it more contagious than other variants — advantages that rely on more than breaking through our prior immunity.
Maybe omicron can produce more copies of itself in a cell? Or maybe it sticks to cells more effectively? Or maybe it’s better at hanging in the air and staying infectious?
“Any of those things would make the virus more contagious,” says Schiffer of Fred Hutchinson.
One key difference emerging with omicron is just how quickly someone who gets infected becomes contagious.
Omicron appears to have a shorter incubation period and that can substantially speed up infections across the population. A study of the Oslo Christmas party outbreak found the incubation period could be about three days, compared to 4.3 days for delta and five days for other variants. A small study from CDC also puts the incubation period at about three days.
“That’s actually a fairly significant difference,” says Schiffer. This would mean there are many more cycles of infections and less time for people who are exposed to take precautions not to expose others.
A mid-December study from Hong Kong has also led scientists to consider that omicron may indeed replicate better in certain cells and therefore have a leg up against delta, at least among the unvaccinated.
Researchers found that omicron multiplied about 70 times faster than delta did in tissue samples from the bronchus — the large airways that lead from the trachea to the lungs. Meanwhile, omicron had much more trouble infecting cells in lung tissue than the original version of the coronavirus that was first identified in Wuhan, China.
“Potentially you could be shedding more virus in your upper respiratory tract than you would be if most of the replication was happening deep in your lungs,” says Angie Rasmussen, a virologist at the University of Saskatchewan.
Like other variants, omicron spreads from the nose and mouth through respiratory droplets at close range and through virus particles that float through the air and can stay suspended for quite a while, especially in places with poor ventilation.
Rasmussen says this data on faster replication in the bronchus tissue “would suggest you might have more virus in those respiratory secretions, which can come out either as mucus if you have a runny nose or certainly can be exhaled as aerosols and droplets.”
Airborne concerns as omicron spreads
If omicron does spread more easily through the air, this faster replication in the bronchus would be one of the two most likely explanations, says Linsey Marr, a professor of engineering at Virginia Tech who studies how viruses transmit in the air. “Infected people are either releasing a lot more virus particles into the air or you can breathe in fewer of them and still become infected — or some combination of those,” she says.
While that Hong Kong study focused on what happens in the lab, a cautionary tale of omicron spreading through the air has also emerged from an isolation facility there.
In a report published in early December, Hong Kong scientists describe how a traveler in quarantine at a hotel infected another person who was staying across the hallway but never actually had face-to-face contact. “Airborne transmission across the corridor” is the most probable explanation, the authors conclude.
“That suggests a very small amount of the virus was able to cause an infection,” says Dr. Michael Klompas, an infectious disease physician and hospital epidemiologist at Brigham and Women’s Hospital. This could mean that omicron requires a smaller dose than previous variants to infect people, although there’s no data yet to establish whether that is true, he says.
While concerning, such early anecdotes need to be interpreted carefully. There are similar instances of airborne transmission with delta, and hotels and other places repurposed to isolate infected travelers are difficult places to turn into quarantine facilities.
“Can we catch omicron more easily through the air than other variants? I don’t think that’s known” says Rasmussen. “What is very clear is that you can catch it more easily, period.”
A somewhat reassuring point
Despite the many unanswered questions about why omicron is so contagious, scientists say it’s important to realize that the coronavirus has not morphed into an entirely new virus.
“The rules haven’t changed, it’s just the margin for error has got a lot smaller,” says Klompas.
When it comes to minimizing your personal risk, the same principles apply: wear a high quality mask like an N95, choose outdoors over indoors if possible and avoid large gatherings with unmasked people, especially if they are not vaccinated.
“These risk reduction measures are additive and you should try to apply as many of them as possible,” says Rasmussen.
Even quick face-to-face interactions appear to be more risky with omicron, in part because people have relied on the vaccines as their only layer of defense, says Chanda. “If you walk into a room full of people and someone is infected, the chances have dramatically increased that you will get the virus” — whether you’re vaccinated or boosted or not.
Copyright 2021 NPR. To see more, visit https://www.npr.org.
9(MDAxODM0MDY4MDEyMTY4NDA3MzI3YjkzMw004))
9(MDAxODM0MDY4MDEyMTY4NDA3MzI3YjkzMw004))








