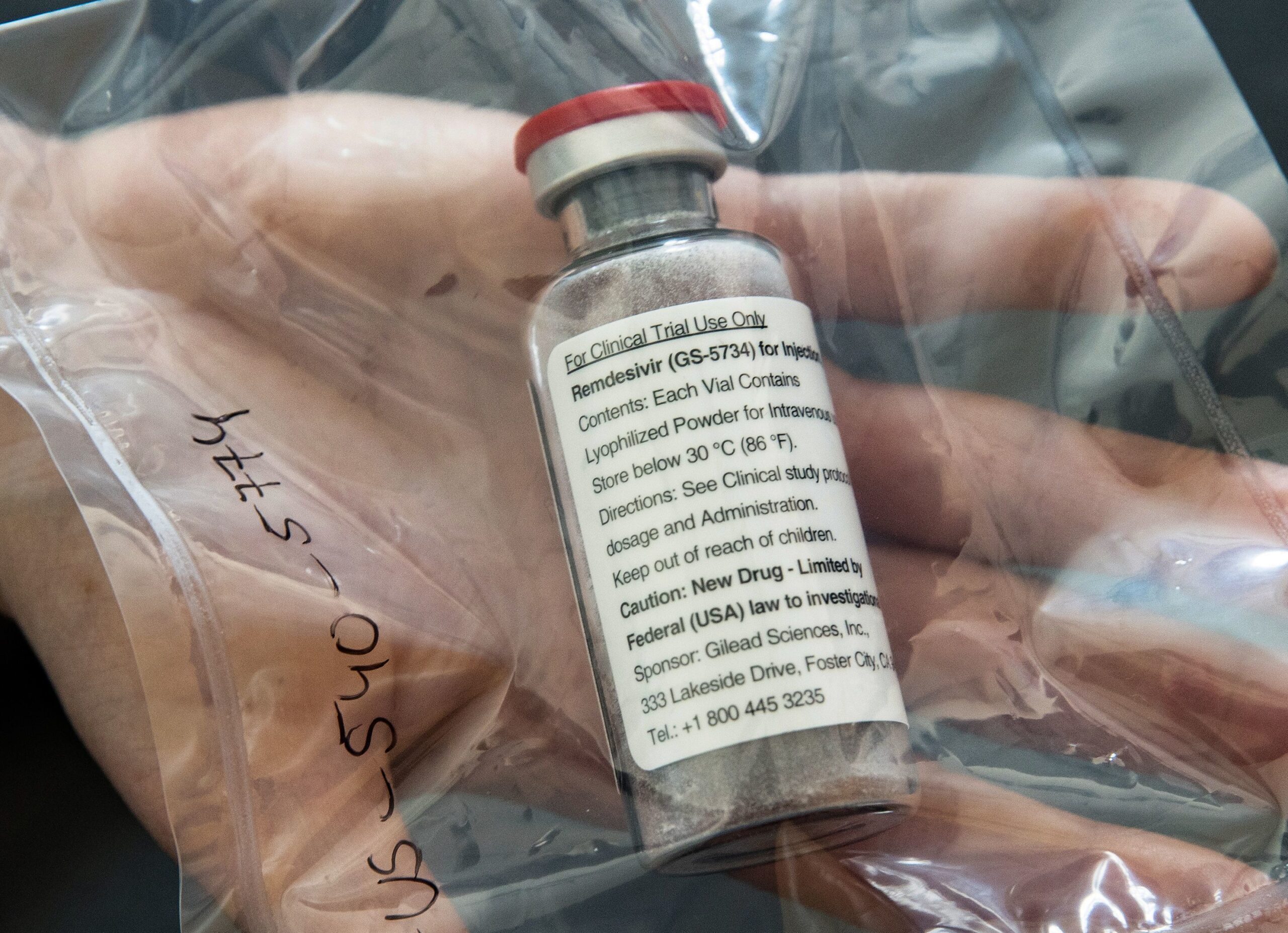
Remdesivir Priced At More Than $3,100 For A Course Of Treatment
Gilead Sciences, maker of the antiviral drug remdesivir, has come up with a price for the COVID-19 treatment that was less than some analysts expected.
ULRICH PERREY / POOL/AFP via Getty Images
The drugmaker behind the experimental COVID-19 treatment remdesivir has announced how much it will charge for the drug, after months of speculation as the company tried to figure out how to balance profit and public health needs in the middle of a pandemic.
In the United States, Gilead Sciences will charge $520 per vial for patients with private insurance, with some government programs getting a lower price. With a double-dose the first day, that comes out to $3,120 for the five-day treatment course. For governments in developed countries outside the U.S., it will cost $390 per vial, or $2,340 for the five-day course. How much uninsured patients would pay is still unclear.
“At the level we have priced remdesivir and with government programs in place, along with additional Gilead assistance as needed, we believe all patients will have access,” Gilead CEO Daniel O’Day said in an open letter posted Monday morning.
Since then, reaction to the price has been mixed.
Some advocacy organizations and members of Congress say Gilead is taking advantage of Americans during a pandemic.
Rep. Lloyd Doggett, D-Texas, called the price “outrageous.”
“Without a taxpayer investment of $99 million, this drug would have been abandoned. It would be on the scrap heap of failures,” he tells NPR. “So it’s the taxpayer who’s really taking the risk here and ought to get the reward of the angel investors that taxpayers are.”
Public Citizen, a nonprofit consumer advocacy group, echoed his remarks with a similar sentiment.
“In an offensive display of hubris and disregard for the public, Gilead has priced at several thousand dollars a drug that should be in the public domain,” Peter Maybarduk, director of Public Citizen’s Access to Medicines Program said in a written statement.
(In a quarterly financial filing, Gilead said its investment in remdesivir for 2020 alone “could be up to $1 billion or more,” much of that money used to scale up manufacturing capacity.)
Still, analysts expected Gilead to set a higher price than the company did.
Geoffrey Porges, an analyst at the investment bank SVB Leerink, said the announced price for the drug offers a “spectacularly good value.”
“It’s unprecedented to price the drug below the medical costs that it’s saving,” Porges said, adding that remdesivir could save up to $40,000 per patient, if it prevents a COVID-19 patient from needing the ICU. And there’s even more value that’s not built into Gilead’s price, he says.
“That ignores the enormous societal value that everybody else gets from making a patient less infectious, for getting a patient back into the community, for getting them back to work sooner,” Porges said. “All of those societal benefits aren’t even considered in this price.”
The Institute for Clinical and Economic Review, or ICER, an influential nonprofit that analyzes drug pricing, said Gilead showed “restraint” and set a “responsible” price.
That said, ICER President Steven Pearson noted that this reasoning assumes remdesivir will eventually be shown to improve COVID-19 survival — something research hasn’t yet proven.
A federally funded study by the National Institute of Allergy and Infectious Diseases published at the end of April indicated that remdesivir can shorten COVID-19 patients’ hospital stays by about four days. But it’s unclear whether the drug also improves survival.
“If further data do not show a clear mortality benefit for remdesivir, then the price of the drug should be dramatically reduced,” Pearson said in his written statement.
The drug price will send a message to companies working on other treatments, vaccines and cures for COVID-19. They have been watching remdesivir closely to find out what kind of reward they might expect for their investments, should their own treatments pan out.
At the announced price, Gilead is still expected to profit from remdesivir sales. That should be encouraging for companies currently investing and developing additional COVID-19 treatments and vaccines.
“Gilead will make a good amount of money selling this product,” Craig Garthwaite, who directs the health care program at Northwestern University’s Kellogg School of Management, told NPR. “And that’s really the return other people have been looking at. In the end, really, the other firms aren’t necessarily looking at the price Gilead charges. What they’re really looking at is, what is the payoff that they get on their investment? ”
Until now, Gilead had been donating doses of remdesivir for use in clinical trials and under the Food and Drug Administration’s emergency use authorization announced in May. The last of the donated supply was distributed by the U.S. Department of Health and Human Services on Monday.
HHS announced that it has “secured” an additional 500,000 treatment courses for the United States — the majority of remdesivir that Gilead plans to manufacture in July, August and September. Although hospitals and insurers will now be charged for the drug, the federal government will continue to manage distribution, which had initially been plagued by confusion when it began in early May.
Overall, the price is less than the highest estimates of what it might be, but more than the lowest ones, Michael Carrier, a professor at Rutgers Law School who specializes in antitrust and pharmaceuticals, told NPR.
“Shareholders aren’t getting the maximum they wanted but that’s to be expected in this environment,” he wrote in an email. “With no simple way to determine what a drug is worth, there will always be plenty to debate!”
9(MDAxODM0MDY4MDEyMTY4NDA3MzI3YjkzMw004))







