Dr. Diana Greene Foster, the demographer behind the study, told NPR in May that the findings show that pregnant people who are unable to get a safe, legal abortion and end up carrying the pregnancy to term will experience long-term physical and economic harm.
“We haven’t become a more generous country that supports low-income mothers,” she added. “And so those outcomes are still the outcomes that people will experience when they are denied a wanted abortion.”
Republican opposition has prevented Congress from passing nationwide measures like federally protected family leave and an extended child tax credit that would expand the social safety net, leaving various forms of support for low-income and vulnerable families up to each state.
Abortion access is now up to states too, after the Supreme Court’s ruling in Dobbs v. Jackson Women’s Health Organization. The case challenged a Mississippi law banning abortions after 15 weeks of pregnancy, which a lower court had ruled unconstitutional. As of mid-August, 14 states have banned abortions entirely, and nearly a dozen others have moved to do the same.
Even before the Dobbs ruling, the 14 states with the most restrictive abortion laws had the worst maternal and child health outcomes in the country, according to an amicus brief filed on behalf of Jackson Women’s Health Organization by the American Public Health Association (APHA), the Guttmacher Institute, the Center for U.S. Policy and hundreds of public health scholars and professionals.
The brief cites poorer maternal and child health outcomes across existing risk measures, including mistimed and unwanted pregnancy, low infant birth weight, infant mortality, child poverty and adverse childhood experiences. (It also notes that Mississippi — at the center of the Dobbs case — ranked last in the Commonwealth Fund‘s 2020 composite score for health system performances on measures including “overall preventable mortality” and “children without appropriate preventive care.”)
These findings are echoed in similar analyses by Evaluating Priorities, the Brookings Institution, the Associated Press, the New York Times and others.
NPR looked at indicators related to maternal and infant health outcomes, as well as policies states have in place to support families, in the 14 states with abortion bans in effect as of early August: Alabama, Arkansas, Georgia, Kentucky, Louisiana, Mississippi, Missouri, Ohio, Oklahoma, South Carolina, South Dakota, Tennessee, Texas and Wisconsin. Here’s what the data show.
It’s harder to get health insurance
Many of the states with abortion bans are the same ones that have chosen not to expand their Medicaid programs, leaving many people without any affordable health insurance options.
A brief refresher: A provision in the Affordable Care Act expanded Medicaid to nearly all American adults with household incomes up to 138% of the federal poverty level, making millions of people newly eligible for coverage. But a 2012 Supreme Court ruling left it up to each state to decide whether to participate.
Thirty-nine states and Washington, D.C., have adopted the Medicaid expansion to date, according to a tracker from the Kaiser Family Foundation. Twelve have not. That creates a coverage gap, leaving more than 2 million Americans without health insurance options because they make too much money to qualify for Medicaid but not enough to be able to get subsidized private coverage in the Affordable Care Act marketplaces.
The 12 states that have not expanded Medicaid are: Alabama, Florida, Georgia, Kansas, Mississippi, North Carolina, South Carolina, South Dakota, Tennessee, Texas, Wisconsin and Wyoming. Eight of them have banned abortion already, while at least two others are attempting to do so.
Medicaid currently finances about 42% of U.S. births. It also covers a majority of births for people with low incomes, amounting to millions of births annually, says Dr. Laurie Zephyrin, an OB-GYN who leads the maternal health work at the Commonwealth Fund.
And Medicaid coverage provides access to all sorts of invaluable services for people of reproductive age, she adds, from prenatal care and case management services to births, doula services and some postpartum care, traditionally up to 60 days after birth.
A provision of the 2021 American Rescue Plan gives all states the option to extend Medicaid postpartum care to up to 12 months after birth. As of mid-August, 33 states and Washington, D.C., either have implemented or plan to implement that extension, according to a tracker from the Kaiser Family Foundation. Abortion restrictive states are less likely to do so, Zephyrin tells NPR.
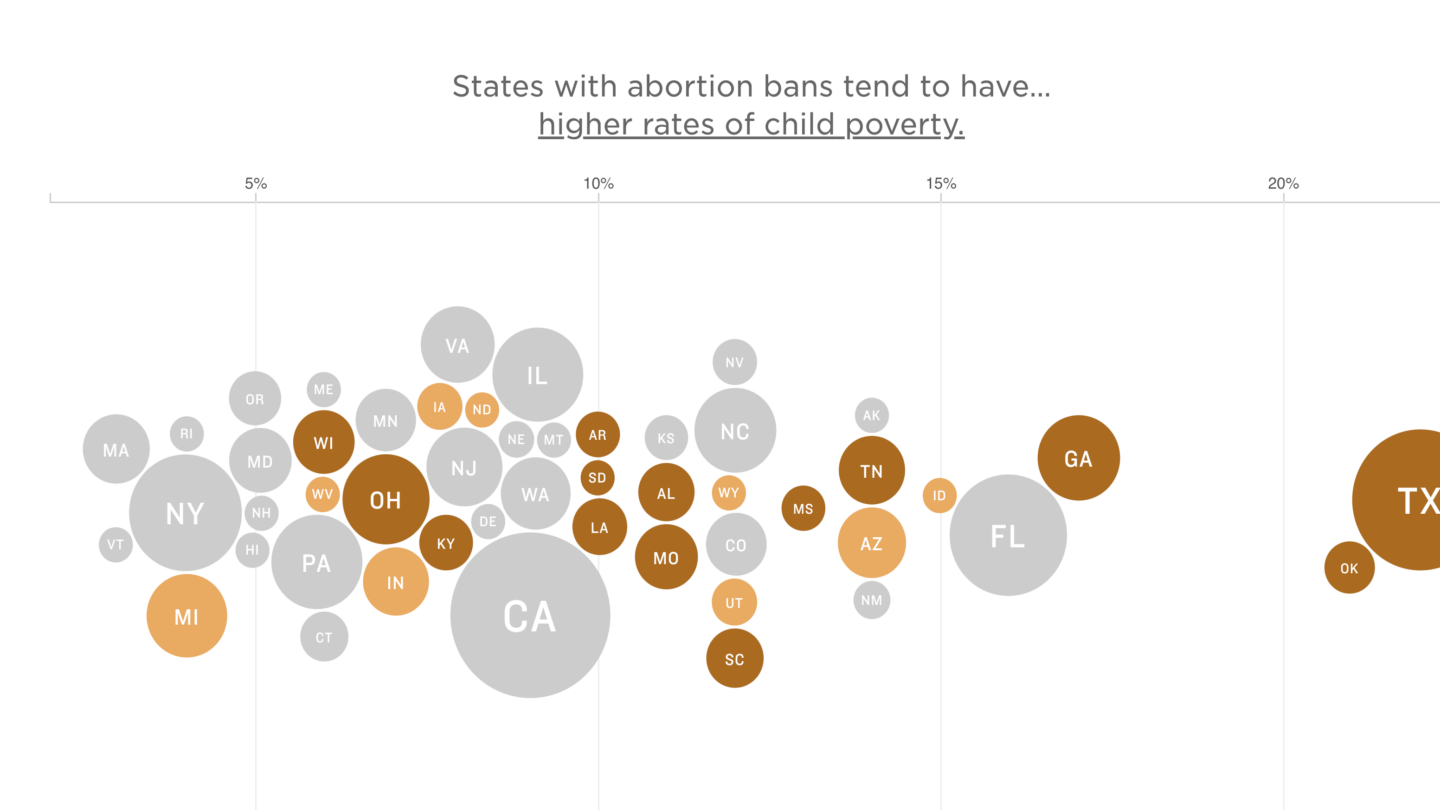
There’s more child poverty
Abortion ban states have some of the highest child poverty rates in the nation, according to a tracker from the Center for American Progress based on U.S. Census data.
Mississippi is the worst-ranked state, coming in at No. 51 with a child poverty rate of 27.9% — meaning that more than one in four children in Mississippi lives in poverty.
More than half of the states in the bottom 10 for child poverty have banned abortion: Alabama, Arkansas, Kentucky, South Carolina, Louisiana, Oklahoma and Mississippi.
The notable outlier is New Mexico, which has the third worst child poverty rate in the country but no major abortion restrictions (and is already seeing an influx of patients from Texas and other nearby states).
More than 150 economists wrote in a Supreme Court amicus brief that access to legal abortion has led to lower rates of children in poverty, as well as mothers attaining higher levels of education and professional occupations. Researchers have drawn those conclusions by comparing the experiences of pregnant people in states that loosened abortion restrictions in the 1960s, compared to those in states that did not.
People who seek abortions are more likely to be living below the poverty line, to already have children and to be experiencing a disruptive life event, all factors that can make it difficult to care for a child, Isabel Sawhill and Morgan Welch of the Brookings Institution pointed out in a recent blog post.
They write that adverse consequences for people who were denied a wanted abortion include financial hardship and health complications as well as, in certain cases, the need to raise a child alone or remain in abusive relationships, all of which will impact their child’s well-being as well as their own.
More babies are born with low birth weight
One measure of infant health is how much a baby weighs at birth.
Low birth weight is defined as when a baby is born weighing less than 5 pounds, 8 ounces. It is most often the result of preterm birth or fetal growth restriction, though there are numerous medical and environmental risk factors.
While some babies with low birth weight are healthy despite their size, others can experience serious health problems, as the nonprofit March of Dimes explains. Some of those may require immediate treatment in the newborn intensive care unit, like brain bleeding or breathing problems, while other conditions could present later in life, such as diabetes and intellectual or developmental disabilities.
CDC data shows that many of the states with the toughest abortion restrictions are also the ones with the highest rates of low birth weight. Five of the bottom six states — Mississippi, Alabama, Georgia, South Carolina and Louisiana — have abortion bans in place, while Wyoming’s near-total abortion ban is delayed by court order.
The problem is especially pervasive among communities of color, with Black babies much more likely than others to weigh less than they should at birth. For comparison, about 1 in 7 Black babies in the U.S. have low birth weight, compared to roughly 1 in 14 white babies.
Some researchers have explored a direct connection between states’ reproductive rights and rates of low birth weight: One 2020 UCLA study found that women living in states with the least restrictive reproductive rights policies had a 7% lower risk of having a child with a low birth rate, and that Black women in those states had an 8% lower risk.
Looking at birth outcomes more broadly, CDC data from 2020 shows that states with abortion restrictions also tend to be the ones with the highest infant mortality rates. More than half of the 10 states with the highest infant mortality rates already have abortion bans in place (Mississippi, Louisiana, Arkansas, Alabama, South Dakota and Ohio). West Virginia has a law banning abortion after 20 weeks, though a judge has blocked enforcement of a ban from 1849.
Pregnant people have less access to care, which threatens their safety
Access to quality maternity care is crucial to the health of mothers and their babies, but is lacking in many parts of the country — and especially in states with restrictive abortion laws.
A 2020 March of Dimes report found that some 2.2 million women of childbearing age live in maternity care deserts, or places where there is no hospital offering obstetric care, no birth center and no obstetric provider. Another 4.8 million live in counties with limited access to maternity care.
An analysis from Stacker.com used federal data to calculate which percentage of a state’s population lives in counties without access to maternal care, in line with March of Dimes’ definition. The highest was Mississippi, where 23.5% of the population lives in a maternal care desert.
All told, eight out of the 10 states with the most people living in maternity care deserts have abortion bans: Mississippi, South Dakota, Arkansas, Missouri, Oklahoma, Alabama, Kentucky and Louisiana. Within the top 15, two other states — Idaho and North Dakota — have abortion bans pending — and another two — Iowa and West Virginia — have bans on hold.
And that lack of maternity care, whether due to lack of services or barriers to accessing it, poses a huge risk. People who do not get prenatal care are five times more likely to die of pregnancy-related causes than those who do, according to the Department of Health and Human Services.
The U.S. as a whole already struggles with maternal mortality, an issue that’s been exacerbated by the pandemic and disproportionately affects people of color.
Even before the Supreme Court overturned Roe, states with more restrictive abortion policies tended to have higher maternal mortality rates, according to data from the CDC.
And a growing body of research has underscored the explicit connection between abortion laws and maternal mortality. For instance, a 2020 study published in the American Journal of Preventive Medicine found that states that enacted laws to restrict abortions based on gestation age increased their maternal mortality rate by 38%.
“We have data already that in the U.S. healthcare system, there’s failure to support the health of women and pregnant people and ensure reproductive health outcomes, particularly for Black and brown communities, for low-income communities, for people living in underserved areas,” says Zephyrin, of the Commonwealth Fund. Abortion bans are “another piece that we’re adding on top of these already existing structural risks and fragility.”
There’s less financial support for families and children
It’s also important to look at what policies and forms of assistance states have in place to support families and children after they’re born.
Many of the most restrictive abortion states make it harder for families to get cash assistance, take time away from work, earn a living wage and access affordable childcare, among other factors.
That’s no coincidence, says Elizabeth Lower-Basch, the director of the income and work supports team at the Center for Law and Social Policy (CLASP). She tells NPR that while many of these states are reluctant to raise taxes or spend more money on social programs (which she says in itself is a legacy of institutional racism), they support banning abortion because – at least until the Dobbs ruling – it was largely symbolic, free of costs as well as consequences.
“Supporting childcare, supporting better prenatal care, supporting better schools, all that actually costs money,” she says. “Voting for an abortion ban, you don’t need to pay for it in the state budget even if it is going to drive up your healthcare or other costs.”
One clear example: Temporary Assistance for Needy Families, or TANF, is harder to come by — both in terms of amount and availability — in states with restrictive abortion policies. (The federal government gives states grants to provide low-income families with financial assistance and other support services, and leaves funding allocation and eligibility for cash assistance largely up to states to decide.)
The Center on Budget and Policy Priorities measures this with its “TANF-to-poverty ratio” (TPR), which calculates how many out of every 100 families in poverty receive TANF assistance each year. In a brief released earlier this year, it said that nationwide number had reached its lowest point in history in 2020 and pointed to states where access is especially limited.
Seven of the 14 states with the lowest TPR’s (of 10 or less) have abortion bans, while several others have bans pending or on hold. The worst-ranking states are Texas, Mississippi, Louisiana and Arkansas, where four out of every 100 families in poverty have access to TANF.
The Center also tracks what percentage of TANF funds each state gives as cash benefits directly to lowest-income families. That number tends to be lower in abortion-restrictive states.
Research associate Diana Azevedo-McCaffrey tells NPR over email that some states, especially those that spend less on basic assistance, use a sizable amount of TANF funds on “other areas,” including after-school programs, youth and children services and short-term benefits to help families in crisis situations.
“While these are worthy and important investments, states should use funding sources other than federal and state TANF funds for them — particularly when states spend so little on providing cash assistance and supporting work for families with the lowest incomes,” Azevedo-McCaffrey added.
Fifteen states spent 10% or less of their TANF funds on basic assistance in 2020, the Center found. Six of them (Alabama, Arkansas, Louisiana, Mississippi, Missouri and Texas) have banned abortions, while two others (Indiana and North Dakota) have bans pending.
“Cash assistance almost might as well not exist in some of these states, it is so hard to access,” Lower-Basch adds.
She said in states with such low benefit levels, and so many hoops to jump through, people may decide it’s not worth the effort or insult to their dignity to apply in the first place. Some require people to apply to a certain number of jobs before considering their applications, and Lower-Basch notes that in today’s economy, someone can find a job during that process and no longer be eligible for TANF, even if their salary is low.
And making a low salary is not an unlikely scenario, especially in restrictive states. Only eight of the 24 states that have banned or are likely to ban abortion have minimum wages above the federal level of $7.25 per hour, Lower-Basch says. She also notes that none of the states that have banned abortion have paid family and medical leave programs — only 11 states and Washington, D.C., do.
In fact, North Dakota passed a law last year banning cities and counties from enacting local paid family leave laws. Lawmakers in the abortion ban states of Oklahoma and Tennessee have introduced — but not passed — such legislation.
Lack of paid leave can pose a sizable problem for working parents, especially if they need to find and pay for childcare for their kids not yet in school. Six states have no publicly funded prekindergarten programs at all — including Idaho, Indiana, South Dakota and Wyoming, which have either banned or moved to ban abortion.
Lower-Basch says that while the trends are “most glaring” in certain states, the U.S. as a whole is not doing enough to support families with children.
What can people do?
The data doesn’t look promising for people forced to carry unwanted pregnancies in abortion-restrictive states. So what options do they have, and what can lawmakers and reproductive rights advocates do?
Lower-Basch says there is very little evidence that people are moving to states to get better economic benefits and opportunities, particularly if they want to stay close to family or don’t have the money or resources to move.
Zephyrin of the Commonwealth Fund agrees, noting that the most marginalized groups are those that will feel the effects of abortion bans the hardest.
“We’re assuming that people that are most affected have the resources — the time, money — to be able to up and travel to another state, and I don’t think that’s a realistic or fair expectation,” she says. “There’s also an importance to think bottom-up in terms of what are ways to get resources to people, to communities on the ground so that some of these impacts can be mitigated.”
That work can include helping people access abortion funds to have more decision-making power over their own bodies, as well as investing in community organizations and health care infrastructure on the ground. There are also top-down solutions, like conducting research and changing policies.
There’s also voting, Lower-Basch adds, noting that many of these states are “not as red as their legislatures” in part due to gerrymandering and voter suppression.
Abortion is shaping up to be a major issue this midterm election season. Kansans recently voted resoundingly to keep abortion legal, but lawmakers elsewhere have campaigned on the false notion that Democrats support abortion until the moment of birth.
Zephyrin stresses the need for urgency.
“We can’t sit in our doom and gloom while people are just experiencing these inequitable outcomes,” she says. “We have to act, and we have to act now.”
Copyright 2022 NPR. To see more, visit https://www.npr.org.
9(MDAxODM0MDY4MDEyMTY4NDA3MzI3YjkzMw004))
9(MDAxODM0MDY4MDEyMTY4NDA3MzI3YjkzMw004))








